Kyphosis (also known as roundback or Kelso’s hunchback) is a condition of excessive forward curvature of the spine, typically in the thoracic segments. This causes the back to develop bowing, which leads to the patient having a slouching posture.
ICD-10 Options Will Be Similar to ICD-9
When ICD-10 goes into effect on Oct. 1, you’ll have specific and simple choices for diagnosis coding of kyphosis.
When submitting a diagnosis of kyphosis, make sure you check for documentation of the underlying cause. This will guide you to the most appropriate code in both ICD-9 and ICD-10.
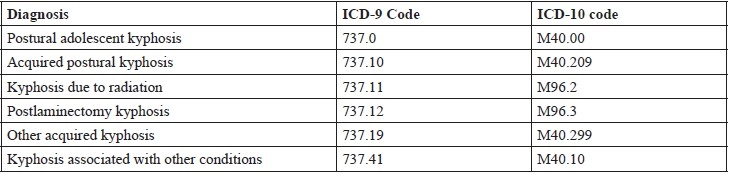
The common ICD-9 and ICD-10 diagnosis codes for kyphosis are as follows:
Understand the Different Types
Kyphosis can be caused by a number of conditions. One of the causes for kyphosis is degeneration, for example, in arthritis. Osteoporosis, vertebral fractures, and vertebral trauma are other common causes for kyphosis. Kyphosis can be acquired due to a persistent bad posture. Kyphosis may occur as a consequence of surgical procedures in the spine, for example laminectomy or as a consequence of exposure to radiation.
Kyphosis may occur due to developmental problems. Scheuermann’s kyphosis is the most classic form of hyperkyphosis and is the result of wedged vertebrae that develop during adolescence. This is a developmental condition, and the cause for this condition is not precisely known.
“Schuermanb’s kyphosis affects younger people, causing an exaggerated forward posture. This is in contrast to aging-related kyphosis that sometime affects the elderly,” explains Gregory Przybylski, MD, director of neurosurgery at the New Jersey Neuroscience Institute, JFK Medical Center, in Edison.
Kyphosis may occur due to other medical conditions. For example, tuberculosis of the spine can cause a structural deformity and result in kyphosis.
“While this deformity is not commonly seen in the U.S. because of a low prevalence of TB, patients who have emigrated from countries where TB infection is endemic may present with this deformity here,” Przybylski says.
Keys to success: As with any condition, the more details your provider documents about the patient’s situation, the more accurate your coding can be. Watch for details about the amount of spinal curvature and any underlying causes to help pinpoint the best diagnosis.
