Outpatient Facility Coding Alert
Just How Many Systems' Review Suffices For a Complete ROS

Question: Instead of checking off boxes in the electronic medical record (EMR) for his review of systems (ROS), the provider just marks “all others negative” instead. Can we count on this for reporting a proper E/M code? Mississippi Subscriber Answer: There is no specific number of systems the provider needs to document alongside the “all others negative” statement. It’s actually left to the provider’s discretion — how many systems can be associated to the complaint. Because the documentation guidelines state, “positive or pertinent negative responses,” if the physician indicated positive or negative for at least one system and checked the “all others negative” box, then he has documented a complete ROS. Caveat: While the decision about ROS is ultimately the physician’s. In any case, he would need to document his findings for at least one system before checking the “all others negative” box for a complete ROS when he hasn’t evaluated any other systems. Naturally, without documentation of positive or negative responses to at least one system, the “all others negative” statement has no value. Another concern could be identifying a consistent pattern of checking the “all others negative” box with no variation in the ROS documentation. It’s important that no two charts look the same to the auditors. Also, if there is only one ROS element in every chart, the medical necessity of treatment comes under question too. Example: If a patient presents with an injury to her arm and three or four ROS are marked (such as respiratory, cardiac, ENT, or abdominal), no auditor will count those systems as pertinent or medically necessary because there aren’t medically necessary reasons to review those systems. Instead, the systems the provider should logically evaluate would be musculoskeletal, skin, and nervous system for peripheral neve, muscular, bony injuries along with laceration of skin.
Related Articles
Outpatient Facility Coding Alert
- MOON Update:
Brace Yourself for Final MOON Implementation
Document reasons for outpatient status to avoid audit hotspot. Worried about complying with the final [...] - JW Modifier Update:
Have You Met the JW Modifier Usage Mandate?
Learn the do’s and don’ts for reporting discarded drugs. Is your facility prepared to report [...] - ICD-10 Update:
Your Coding Accuracy Is Under Fire
Take stock, and run a claims audit before it’s too late. Are you finding it [...] - You Be the Coder:
Just How Many Systems' Review Suffices For a Complete ROS
Question: Instead of checking off boxes in the electronic medical record (EMR) for his review of [...] - Reader Question:
Don't Go by Appendix B of AMA's CPT® 2017 For Moderate Sedation
Question: Going by AMA’s CPT® 2017 Appendix B, “Summary of Additions, Deletions, and Revisions,” one should [...] - Reader Question:
Sharpen Your I & D Coding Skills
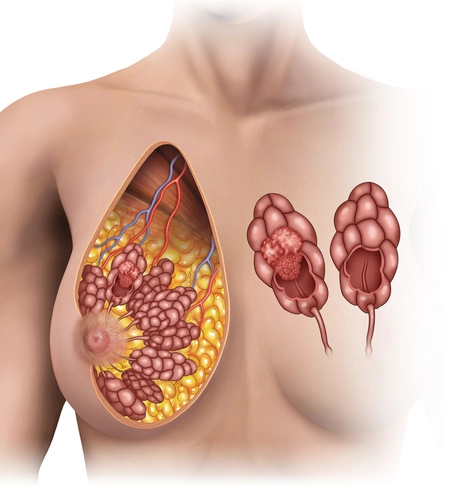
Question: A new patient comes to the office with complaints of acute pain and tenderness in [...]