Outpatient Facility Coding Alert
Keep Up On PFS by Building a Comprehensive Understanding of RVUs

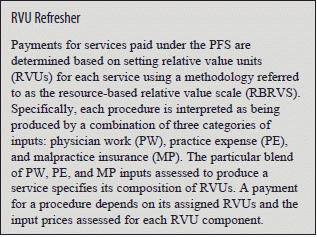
The Centers for Medicare and Medicaid Services (CMS) pays physicians for their services based on submission of a claim according to the Physician Fee Schedule (PFS).
Medicare pays for physician services based on a list of services and their payment rates. Under the PFS, every physician service corresponds to a specific procedure code within the Healthcare Common Procedure Coding System (HCPCS).
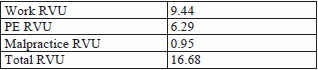
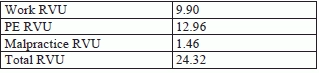
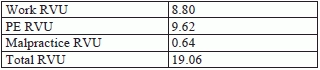
Since 1992, CMS has relied on the RBRVS system to determine the fee for each procedure. In the RBRVS system, payments for each service depend on the relative amounts of inputs required to perform the procedure. These inputs include the amount of physician work needed to provide a medical service, expenses related to maintaining a practice, and malpractice insurance costs. Here are few examples of RVU breakup of “National Facility” charges:
i. When you are coding for incision in bone cortex in a foot (28005, Incision, bone cortex [e.g., osteomyelitis or bone abscess], foot)
ii. When you are coding for lengthening of palate with Island flap (42227, Lengthening of palate, with island flap)
iii. When you are coding for repair of retinal detachment, 1 or more sessions (67101, Repair of retinal detachment, 1 or more sessions; cryotherapy or diathermy, with or without drainage of subretinal fluid)
Higher RVU, higher input: CMS estimates the quantity of inputs required to provide these services under the PFS using the RVUs based on physician workload, physician expense, and malpractice costs, respectively. Higher RVU levels indicate that the service requires more inputs.
Learn About Conversion Factors and Budget Neutrality
The conversion factor converts the relative value units into an actual dollar amount. The dollar multiplier (CF) is updated on an annual basis according to a formula specified by statute. Congress has the ability to override the statutorily defined formula, as it has done in the past. Note that the CF is adjusted for budget neutrality.
CMS is prohibited from changing its overall budget by more than $20 million. Should RVUs shift in such a way that the CMS budget is impacted by over $20 million, CMS must use a budget neutrality factor to bring its total payments back in line.
Know the Geographical Implications on RVUs
Geographic Practice Cost Indices (GPCIs) measure regional variation in the price of each of the three input categories. In essence, GPCIs increase the price associated with an RVU in high cost regions and decrease the price associated with an RVU in low cost regions. GPCIs are budget neutral and do not affect aggregate payment levels; rather, they reallocate payment rates by locality to reflect regional variation in relative input prices.
For example, a PE GPCI of 1.2 indicates that practice expenses in that area are 20 percent above the national average, whereas a PE GPCI of 0.8 indicates that practices expenses in that area are 20 percent below the national average. The three GPCIs are calculated for 89 localities. The localities are defined alternatively by state boundaries (e.g., Wisconsin), metropolitan statistical areas (MSAs) (e.g., Metropolitan St. Louis, MO), portions of an MSA (e.g., Manhattan), or rest-of-state area which exclude metropolitan areas (e.g., Rest of Missouri).
Using the RVUs, GPCIs, and a conversion factor (CF), one can calculate the PFS payment for any service in any locality. The CF translates the sum of the GPCI-adjusted RVUs from RVUs into dollars.
The equation below shows how the PW, PE, and MP GPCIs combine with the three RVUs and the CF to establish a Medicare physician payment for any service (K) in a locality.
Payment K L = {[GPCI PW, L × RVU PW, K] + [GPCI PE, L × RVU PE, K] + [GPCI MP, L × RVU MP, K]
Thus, each CPT® code has an RVU assigned to it which, when multiplied by the conversion factor (CF) and a geographical adjustment (GPCI), creates the compensation level for a particular service.
Related Articles
Outpatient Facility Coding Alert
- Billing Strategy:
Pay Attention to the Payer-Provider Relationship
Good relations with payers can help you better manage hospital accounts receivables. The physician-patient relationship [...] - ICD 10 Update:
You Don't Need to Fret Over Numerous Codes for Strep Throat
Choose one of three options for an appropriate description. You won’t have to select from [...] - RVUs Refresher:
Keep Up On PFS by Building a Comprehensive Understanding of RVUs
Break down the components of your payment. The Centers for Medicare and Medicaid Services (CMS) [...] - Reimbursement:
Strengthen Your Consolidated Bills With These 4 Tips
Read on to know how to negotiate SNF patient cases. Your physician performs services for [...] - You Be the Coder:
Know When to Use 31622 and 31623
Question: My doctor wants me to bill 31623 and 31622 for services during the same encounter, [...] - Reader Questions:
Clear Calcific Band Keratopathy With 371.43
Question: I have a patient with extreme calcific band keratopathy. Is there a more specific ICD-9 [...] - Reader Questions:
Step Away From Traditional "Fee-For-Service" Arrangement
Question: When a surgery being performed in an ASC under general anesthesia, can the ASC bill [...] - Reader Questions:
Report 28299 for Bunion Deformity
Question: Can CPT® code 28299 be used for a patient that does not have a bunion [...] - Reader Questions:
Depend on Number and Nature of the Nails to Choose Between 11719, 11721, 11720
Question: What CPT® code is best for cutting and filing ten toenails? Indiana Subscriber Answer: The answer [...] - Reader Questions:
Choose 45378 When Colonoscopy is Used as Diagnostic Method
Question: Our physician performed a colonoscopy for a rectal bleed on a Medicare patient. The patient [...]




