Minimize Pressure of Pressure Ulcer Coding, Use these 4 Pointers

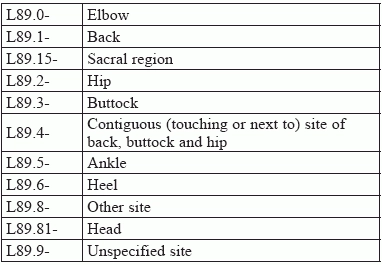
Look for site, severity, and more. When your surgeon treats pressure ulcers, you'll need to focus your diagnosis coding if you want to demonstrate medical necessity for the procedure. Also called decubitus ulcers or "bed sores," surgeons might debride the area, allowing the wound to stay opento heal, which you'd report with codes in the range 11042-+11047 (Debridement ...). This process is called closure by secondary intention, versus primary intention, which involves some sort of definitive, active closure. Alternatively, the surgeon might excise the ulcer and close the wound, which would direct you to codes 15920-15999 (Excision ... pressure ulcer ...). Either way, you need the following four expert tips to make sure you're correctly reporting diagnosis codes on your claims: Tip 1: Determine if Ulcer Involves Gangrene If your surgeon's notes indicate the patient has gangrene, you'll need to code that first before you dig into the pressure ulcer codes. ICD-10-CM directs you tocode the condition with I96 (Gangrene, not elsewhereclassified) and sequence it before the specified pressure ulcer. Tip 2: Identify Pressure Ulcer Anatomic Site Surgeons need to carefully document the location of decubitus ulcer(s) treated in a single operative session, because anatomic site is the starting point for accurate coding. ICD-10 breaks down pressure ulcer sites in the following way: Be specific: The fourth digit of L89.- indicates the pressure ulcer anatomic site, such as hip or heel. You should always report the most specific ICD-10 code supported by your surgeon's documentation. That means you should reserve L89.9- (Pressure ulcer of unspecified site) for cases when the surgeon does not document where the pressure ulcer is at all. That should be a rare occurrence, but use of L89.9- is on the rise because many physicians have this as their default code choice in their electronic health records (EHR). "Using L89.9- could cause problems for treatment and care reimbursement, because certain care is more appropriate for feet as opposed to the sacrum, hips, or other locations that pressure ulcers may appear," advises Marcella Bucknam, CPC, CCS-P, COC, CCS, CPC-P, CPC-I, CCC, COBGC, revenue cycle analyst with Klickitat Valley Health in Goldendale, Washington. "Coders should also include the stage, if possible, because that will also support the need for different treatments for the wounds." As we move to more outcomes-based care, correctly identifying the pressure ulcer site will become even more important for coverage and reimbursement. 'Other' is different: Reporting L89.89- (Pressure ulcer of other site) is not the same as coding L89.9-. "'Other site' means that the provider has indicated where the ulcer is, but there is no specific code under L89.- that specifies the site documented," says Melanie Witt, RN, CPC, MA, an independent coding expert based in Guadalupita, New Mexico. Problem: Patients often present with pressure ulcers at multiple sites, which can complicate coding. Look at the op note to determine which site(s) your surgeon is treating in the session at hand. If the note documents multiple sites, you should sequence the codes by reporting the most severe pressure ulcer first. See Tip 4 to understand how you determine "severity." Tip 3: Code for Laterality ICD-10 further specifies the L89.- codes by laterality, which means that you can choose between right, left, and unspecified anatomic areas of most sites. There are no bilateral codes, which means that you must separately code right and left sides when pressure ulcers equally affect both sides of regions such as the hips and buttocks. The fifth digit of the L89 codes indicates laterality, such as the following: Some sites give even more specific choices, such as the following fifth-digit options for pressure ulcers of the back: Tip 4: Code for Severity ICD-10 categorizes pressure ulcers by degrees of severity, known as stages. The stages correlate to the depth of the tissue damage. The sixth and final character of L89 codes describes the stage of the ulcer. ICD-10 provides descriptions of each stage, as follows: Clarify: Unstageable is not the same as unspecified. In some cases, the surgeon can't determine depth or stage of the wound because slough and/or eschar cover the wound bed, often enabling the wound to heal. For that reason, the surgeon may choose not to remove the covering just to determine the stage and would designate the pressure ulcer as "unstageable." On the other hand, "unspecified" means that the op report gives no indication about the stage of the pressure ulcer. Read more: For more details about the National Pressure Ulcer Staging System, go to www.ncbi.nlm.nih.gov/books/NBK2650/pdf/Bookshelf_NBK2650.pdf.