Work Out 3 Unique Cataract Coding Cases
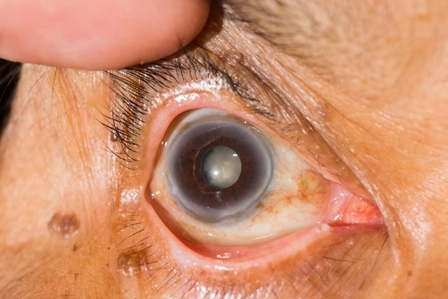
See how well you understand cataract bundling rules. Cataract services can be nuanced and complex, and the hefty reimbursement for these procedures means you don’t want to make any mistakes throughout the coding process. Utilize this quick quiz set to test your knowledge and skills with three cataract coding scenarios. Question 1: Unplanned Vitrectomy Question: During the course of a cataract removal, the vitreous collapses and the ophthalmologist finds it necessary to perform a vitrectomy. Can you code separately for the vitrectomy? Answer: The answer depends on whether the vitreous collapse was an iatrogenic (inadvertently introduced) complication. Ophthalmologists often have to perform a vitrectomy during cataract surgery due to vitreous collapse in the course of removing a dense, senile cataract. In these cases, Medicare considers the vitrectomy a component of the cataract surgery, and thus not separately payable. The National Correct Coding Initiative (NCCI, or CCI) bundles vitrectomy codes 67005 (Removal of vitreous, anterior approach [open sky technique or limbal incision]; partial removal) and 67010 (... subtotal removal with mechanical vitrectomy) into cataract surgery codes 66982 (Extracapsular cataract removal with insertion of intraocular lens prosthesis [one stage procedure], manual or mechanical technique, complex ...) and 66984 (Extracapsular cataract removal with insertion of intraocular lens prosthesis [one stage procedure], manual or mechanical technique [e.g., irrigation and aspiration or phacoemulsification]). Rationale: When procedures are performed together that are basically the same, or performed on the same site but are qualified by an increased level of complexity, the less extensive procedure is included in the more extensive procedure. Exception: If a prolapsed vitreous exists and is known in advance —and documented in the patient medical record — it is not considered a complication of the cataract surgery. Therefore, the physician who plans to perform a vitrectomy during the same operative session of cataract surgery may code separately for the vitrectomy using modifier 59 (Distinct procedural service): 67005-59 or 67010-59, assuming the documentation supports the code and demonstrates the separate and distinct nature of the services. Key: Documentation and diagnosis codes can aid your reimbursement. Use H43.0x (Vitreous prolapse…) for the vitrectomy and the appropriate cataract diagnosis for the cataract removal. Be prepared to provide documentation in case you receive denials when using the cataract and vitrectomy codes together, despite using modifier 59. Payers are aware of the potential for abuse of 59 and may want you to go through the review process to prove you’ve met the definition of “distinct procedural service.” Provide the chart notes to show that you knew about the vitreous collapse in advance and that you made plans to repair it prior to the surgical session of another service. Also, you should provide the operative report with clear documentation showing that there was another condition, besides the cataract surgery, that made the vitrectomy medically necessary. Question 2: IOL Insertion on Separate Eye Question: On January 1, an ophthalmologist performs an extracapsular cataract removal with intraocular lens (IOL) insertion on a patient’s right eye. One month later, on February 1, he performs the same surgery on the patient’s left eye. The cataract procedure, 66984, has a 90-day global period. To report 66984 performed on the left eye a month after the original surgery, you’ll need a modifier — but which one? Answer: Because the two surgeries seem related, you may be tempted to append modifier 78 (Unplanned return to the operating/procedure room by the same physician or other qualified health care professional following initial procedure for a related procedure during the postoperative period) to the second cataract surgery, but that would be a mistake. The surgery in the left eye is considered unrelated to the initial surgery in the right eye. The best option here would be modifier 79 (Unrelated procedure or service by the same physician or other qualified health care professional during the postoperative period). Remember also to append the “side” modifiers, LT (Left side) or RT (Right side), to demonstrate that the ophthalmologist performed the procedures on opposite eyes. Report 66984-79-LT for the second cataract surgery. Question 3: Related Procedures Question: On April 15, the patient from Question #2 presents with after-cataracts in his left eye. The ophthalmologist incises the posterior capsule with a YAG laser. The global period for the original cataract surgery expired before April 15. Do you need to append a modifier to the YAG capsulotomy? If so, which modifier? Answer: In this case, the global period for 66984-RT is over — but the patient is still in the postoperative period for 66984-LT. When the ophthalmologist performed 66984 on the left eye on February 1, a new 90-day global period started, which would end on May 1. Code 66821-78-LT (Discission of secondary membranous cataract (opacified posterior lens capsule and/or anterior hyaloid); laser surgery [eg, YAG laser] [1 or more stages]; Unplanned return to the operating/procedure room by the same physician or other qualified or other qualified health care professional following initial procedure for a related procedure during the postoperative period; Left side). If the patient also had after-cataracts in his right eye, you would code 66821-79-RT. That procedure, although occurring within the global period of 66984-LT, is unrelated to it, warranting the use of modifier 79. The global period for the related procedure, 66984-RT, would already have expired. If the YAG laser is performed in the private practice office setting during the global period of the eye surgery, it is only a billable service if the practice has a dedicated laser suite or surgical suite, and the service is performed in that dedicated suite, says Gina Vanderwall, OCS, CPC, CPPM, financial counselor with Finger Lakes Ophthalmology in Canandaigua, New York. “It is not billable if the YAG is taken into the examination room and performed in that manner. Make sure the provider documents that the patient was taken to the minor OR, laser suite, surgical suite, etc., in their operative note.”