Otolaryngology Coding Alert
You Be the Coder:
Know When Modifier 52 Works for 69210 Billing
Published on Mon Jun 14, 2021

You’ve reached your limit of free articles. Already a subscriber? Log in.
Not a subscriber? Subscribe today to continue reading this article. Plus, you’ll get:
- Simple explanations of current healthcare regulations and payer programs
- Real-world reporting scenarios solved by our expert coders
- Industry news, such as MAC and RAC activities, the OIG Work Plan, and CERT reports
- Instant access to every article ever published in Revenue Cycle Insider
- 6 annual AAPC-approved CEUs
- The latest updates for CPT®, ICD-10-CM, HCPCS Level II, NCCI edits, modifiers, compliance, technology, practice management, and more
Related Articles
Other Articles in this issue of
Otolaryngology Coding Alert
- ICD-10-CM:
Master These Tricky Malunion Fx 7th Character Reporting Guidelines
Do you know the difference between seventh characters A and P? Find out. Fracture coding [...] - Guidelines:
Discern Between Manifestation, Sequela Diagnoses With 2 Examples
See what the guidelines say for COVID-19 manifestation reporting. While manifestation and sequela diagnoses are [...] - Modifiers:
Compare, Contrast Modifiers 52 and 53 for Terminated Surgeries
Here’s how to handle a provider-planned reduction in service. When your otolaryngologist has to stop [...] - You Be the Coder:
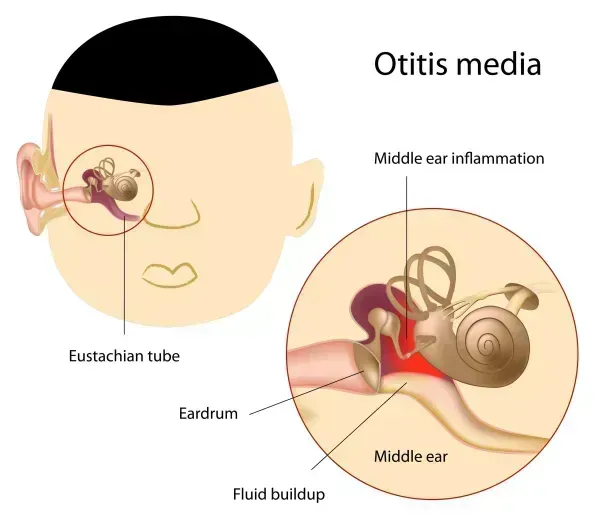
Know When Modifier 52 Works for 69210 Billing
Question: A patient arrived for an office visit for removal of cerumen in the right [...] - Reader Questions:
Include Ventilating Tube Removal in E/M Service
Question: Our provider removed a ventilating tube using a binocular microscope during an office visit. [...] - Reader Questions:
Follow These 2021 E/M Guidelines for Parent Consultations
Question: The 2021 revisions to the office/outpatient evaluation and management (E/M) codes no longer contain [...] - Reader Questions:
Following This Recommended Consultation Coding Advice
Question: Our physician offered consultation services to a patient who was in treatment with another [...]
View All