Otolaryngology Coding Alert
Thorough Documentation Can Help Battle Endoscopy Denials
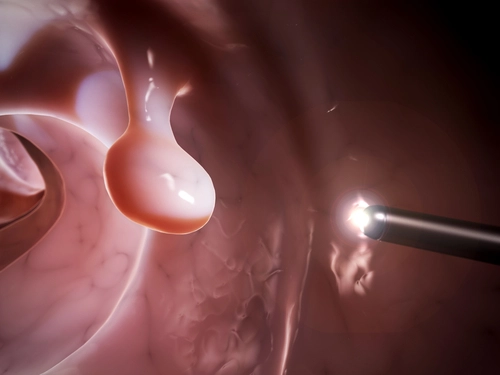
Question: Some of our physicians have been receiving denials for not documenting nasal endoscopies well enough. What should we be including in the notes?
Kansas Subscriber
Answer: Many practices (and some EMR systems) have to help the physicians complete a full report. Complete documentation of a fiberoptic and/or nasal endoscopy procedure with a distinct procedure report which should include:
Think of this procedure not as an office operative note that is included in the patient’s chart (paper or electronic).
Providers might also be asked to state within the physical exam or in the indication section the reason why the nasal endoscopy was medically necessary (i.e. indirect exam findings warranted further direct exam by scope due to inadequate visualization via manual exam, or gag reflex makes indirect exam impossible, etc.).
Many payers have internal edits in place to capture claims being submitted by physicians that may alert them to over billing. If something gets “flagged” in their system, the payer denies the claim for medical necessity and asks the practice to submit a reconsideration with medical notes. Your payer might be invoking a similar edit; it's an automatic way to basically request medical notes. Usually once the notes are submitted the claims get paid.
Don’t forget: Your notes are put under a microscope once you have to send them in on appeal in order to be paid what your physicians have earned. Make sure that all of your documentation can stand -up to full scrutiny.
Related Articles
Otolaryngology Coding Alert
- Coding Edits:
Newest CCI Pairs Bundle IV Infusions With Thousands of Procedures
But – The changes won’t alter your coding much. The latest version of Correct Coding [...] - Clip N Save:
Let This Chart Help You Keep Inferior Turbinate Codes Straight
Now it’s easy to know how to report each procedure. - Procedure Focus:
Remember 3 Checkpoints for Inferior Turbinate Procedures
Plus: Here’s how to handle middle turbinate coding. The nose has three turbinates (inferior, middle [...] - ICD-10:
Stick With a Single Code for Unspecified Sensorineural Hearing Loss
The updated descriptor is basically the same. One diagnosis that hasn’t had much change in [...] - You Be the Coder:
Coding Grafts During Tympanoplasty
Question: I am confused on the graft codes during tympanoplasty. I know the graft is included [...] - Reader Question:
Choose 69220 for Cholesteatoma Debridement
Question: Our physician debrided a cholesteatoma in the external ear canal. How is this coded? Missouri [...] - Reader Question:
Study Options for Post-Tonsillectomy Hemorrhage Diagnosis
Question: I am having difficulty finding the appropriate ICD-10 code for post-tonsillectomy hemorrhage. What do you [...] - Reader Question:
Mine the Details Before Coding Co-Surgery
Question: I am receiving denials for code 62165 endoscopic pituitary tumor excision when my ENT and [...] - Reader Question:
Laterality and Approach Determine PCS Code for 69436
Question: I can’t find the 2016 ICD-10 PCS code for 69436. Can you help? West Virginia [...] - Reader Question:
Thorough Documentation Can Help Battle Endoscopy Denials
Question: Some of our physicians have been receiving denials for not documenting nasal endoscopies well enough. [...] - Reader Question:
'Diagnostic' Is the Key to Submitting Multiple Scopes
Question: The otolaryngologist performed a direct laryngoscopy, direct bronchoscopy, and rigid transoral esophagoscopy during the same [...]