Note Insurer to Keep HPI Counts on Point
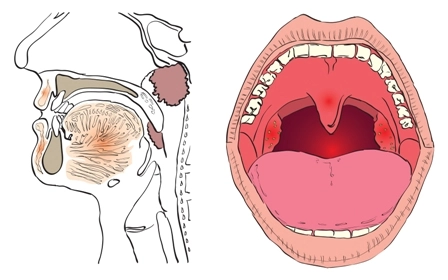
Question: An established patient reports to the otolaryngologist with a chief complaint of throat pain. Notes indicate that the otolaryngologist asked the patient the location of the pain, how severe the pain is, how long the pain has lasted, and whether the pain is accompanied by any other issues. Which level of history of present illness (HPI) is this encounter?
Arkansas Subscriber
Answer: It depends on the insurer’s policy, as your encounter lies right on the line between two HPI levels.
The rules: CPT® lists seven elements on its HPI list: location, quality, severity, timing, context, modifying factors, associated signs and symptoms), but Medicare includes duration as an eighth element. Depending on which rules the payer follows, your otolaryngologist reviewed three or four systems. Three for a Medicare payer, and four for a payer that’s governed by CPT® guidelines.
Your claim: If you’re reporting the claim to a Medicare-observant payer, your otolaryngologist performed an extended HPI. Conversely, if you’re reporting the claim for a patient insured by private payers, your otolaryngologist performed a brief HPI.
Most payers accept duration as an HPI element. If you have a payer who is disallowing duration, you might be able to win on appeal once you show how relevant the duration is to understanding the problem’s history. Without duration, the HPI is an incomplete picture, so be sure to appeal if a payer denies duration as an HPI element.
Why it matters: CPT® rules dictate that brief HPI can only be part of problem-focused or expanded problem-focused history; therefore, brief HPI can support the following office visit E/Ms:
If you’ve got an extended HPI, it might mean that you can code for a detailed or comprehensive history; therefore, extended HPI can support the following office visit E/Ms:
Remember: An extended HPI does not guarantee a higher-level E/M code; it only makes reporting these E/M codes possible. Always keep your E/M coding within the scope of medical necessity of the patient’s presenting problem. If the otolaryngologist performs a comprehensive history and detailed exam on a relatively simple problem — such as an earache — you will be hard-pressed to justify more than a level-two or -three E/M for the encounter. The patient would have to have significant co-morbidities, and possible failed treatments and recurrences, to justify a higher-level E/M.
Warning: Payers are always on the lookout for artificially inflated HPI levels on claims, as they can affect the level of evaluation and management (E/M) service you code. The physician should only cover HPI elements that are relevant to the chief complaint. Listing irrelevant HPI elements to increase levels could raise red flags with payers.