Looking For Modifiers For Procedures By Two Different Specialists? Think Again
Question: Our surgeon recently performed a tongue biopsy on a patient while the patient was in the operating room for a gastroenterological procedure. When our clinician first saw the patient, she was too ill to biopsy this lesion, but when stabilized, our gastroenterologist took her to the OR and called us in to perform this biopsy. What code should we report for the procedure?Should we append modifier 62 or 80 to this service?
Texas Subscriber
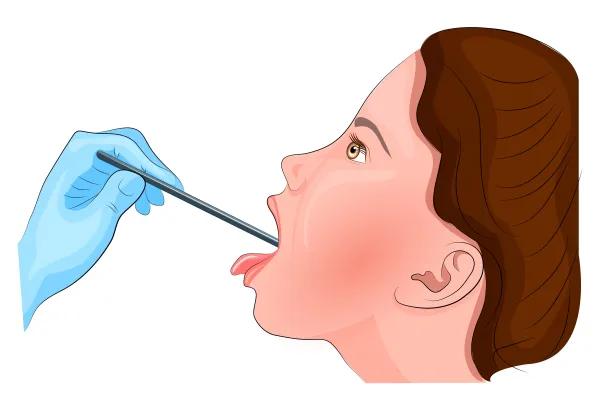
Answer: Since your surgeon performed a biopsy of the tongue, you will have to report one of these two codes depending on the anatomical area of the tongue where your clinician performed the procedure:
Your surgeon performed the tongue biopsy and the gastroenterologist performed a totally different procedure altogether. So, for the biopsy part of the procedure, you will be reporting one of the two above mentioned codes under your surgeon’s provider identifier number while your gastroenterologist will be making a separate claim for his part of the procedure using his provider identifier number.
So, as both the procedures were totally separate, you will just have to make two separate claims. In either of the claim, you do not have to append modifier 62 (Two surgeons) or modifier 80 (Assistant surgeon) to the procedural codes that you are claiming for.
Your surgeon performed side-by-side surgeries with the gastroenterologist. Since they were not part of the same procedure, neither surgeons did not perform cosurgery (modifier 62) nor did your surgeon assist with the GIs procedure (modifier 80).




