Oral Surgery Coding & Reimbursement Alert
Decide From Two Options When Reporting Diagnosis of Xerostomia
Hint: Don’t forget to report additional codes to identify alcohol or tobacco use.
When your clinician diagnoses xerostomia (dryness of the mouth), you will have check the cause for the disturbance in salivary secretion as this has a direct bearing on the code that you will select for the condition.
When your oral surgeon arrives at a diagnosis of xerostomia, you have two code choices in ICD-10 to choose from. The two code choices that you have include:
-
K11.7 – Disturbances of salivary secretion
-
R68.2 – Dry mouth, unspecified.
Even though ICD-10 gives you two options, you will have to report a diagnosis of xerostomia with K11.7 as this is a more specific code to report the condition rather than using R68.2. If your clinician reports the occurrence of dry mouth as a symptom (such as in Sjogren’s syndrome), then you report the dry mouth with R68.2.
When reporting any conditions that are reported under the parent code K11.-, you are also supposed to report additional codes that will identify alcohol abuse and dependence (F10.-); exposure to environmental tobacco smoke (Z77.22); history of tobacco use (Z87.891); occupational exposure to environmental tobacco smoke (Z57.31); tobacco dependence (F17.-) or tobacco use (Z72.0). So if your surgeon identifies a history of tobacco use or dependence or alcohol use or dependence, you will need to report it with additional codes as mentioned.
Caveat: You should note that K11.7 is a generalized code for any disturbances of salivary secretion and is not a specific code for “xerostomia” alone. So, you can use K11.7 for other disturbances of salivary secretion too. So, for instance, if your clinician arrives at a diagnosis of “ptyalism” or “hypoptyalism,” you will code these conditions also with K11.7 as these conditions are also caused due to disturbances of salivary secretions.
In cases where radiation treatment causes xerostomia, you would report the appropriate head and neck cancer codes in addition to reporting K11.7 and L59.9 (Disorder of the skin and subcutaneous tissue related to radiation, unspecified). Check your payer policies to get the final word on which codes they require on the claim for payment.
Look Through These Basics Briefly
Documentation spotlight: Some of the common findings that your clinician will record when he arrives at a diagnosis of xerostomia will include severe dryness of the mouth that is causing the patient to have difficulties in tasting, chewing, swallowing, and speaking. Some patients might complain of experiencing opportunistic infections of the oral cavity, burning sensations in the mouth, alterations to sensations of taste and smell and bad breath. In addition, some patients might complain of experiencing severe feelings of thirst and may also complain of dryness of the lips and development of cracked lips and sores at the angles of the mouth (canker sores).
Upon examination, your clinician might note that the patient has dryness of the oral cavity and the lips. He also might note that due to the dryness of the mouth, the tongue has a tendency to stick to the palate and the patient has stickiness of the lips too. He might also note that the examination gloves or the mirror that he used to examine the patient is also sticking to the mucosal tissues due to the excessive dryness that the patient is experiencing.
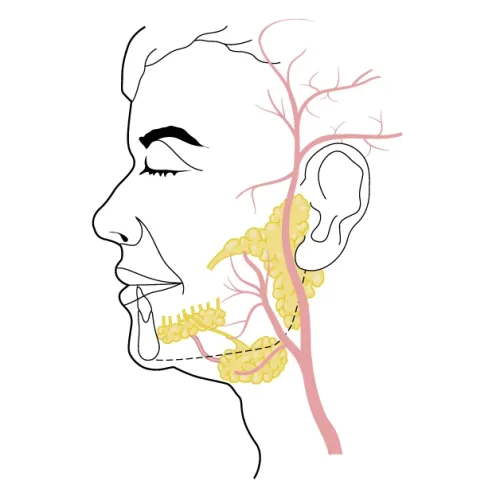
Your clinician might also note that saliva cannot be expressed from the orifice of the parotid gland duct upon stimulation and the saliva present in the oral cavity is quite thick in composition. There might be signs and symptoms of acute sialoadenitis with inflammation and swelling of salivary glands. Your clinician might also note that the patient’s tongue has an atrophied appearance with presence of erythema. Your clinician might also note that the patient has a higher incidence of “caries” and “gingival inflammation” that can be correlated to the dryness of the mouth.
Tests: In most cases, your clinician will identify the diagnosis of “xerostomia” based on history, signs and symptoms, and on the observations of clinical examination. However, he might undertake certain tests to confirm the diagnosis and to check if any systemic conditions are causing the condition.
Your clinician might order for routine blood tests and urine tests to help rule out the possibility of systemic conditions that might be the cause for the xerostomia. In addition, your clinician might order for investigative studies like chest x-ray, ultrasound studies or an MRI to help rule out systemic conditions like Sjogren’s syndrome, sarcoidosis or tumors as being the cause for the xerostomia.
Apart from these tests, your clinician might opt to undertake a biopsy of the salivary glands to check the functioning of the glands and to see if there are any conditions that are affecting the glands. To check the flow rate of saliva, your clinician might undertake a simple office procedure called “sialometry.” By this test, your clinician will collect saliva, produced either by stimulation using citric acid or without any stimulation, into a container that will help him calculate the flow rate of the saliva.
Your clinician might also want to check if there is any blockage of the salivary gland ducts. For this your clinician might undertake a “sialography” wherein your clinician will inject a radiographic dye and undertake an x-ray to see if there is any blockage of flow of the saliva in the gland ducts.
Based on history, signs and symptoms, and results of tests and histological tests, your clinician will arrive at a diagnosis of xerostomia.
Related Articles
Oral Surgery Coding & Reimbursement Alert
- CPT® Coding Strategies:
Perfect Your Dentoalveolar Excision Coding With These 3 Useful Tips
Hint: Don’t leave $240 on the table by failure to identify right type of repair. [...] - ICD-10 Coding:
Decide From Two Options When Reporting Diagnosis of Xerostomia
Hint: Don’t forget to report additional codes to identify alcohol or tobacco use. When your [...] - Medicare News:
Be Informed About OIG's Takedown of Those Receiving Kickbacks
Latest technology and data analysis helps capture more than 300 offenders. If you are constantly [...] - Medicare News:
Get a Thorough Understanding About Kickbacks and Self-Referrals
Don’t raise any red flags by falling into these loops inadvertently. As the Office of [...] - You Be the Coder:
Get Clarity on Reporting Wilke Procedure With Submandibular Excision
Question: Our surgeon recently performed Wilke’s type of surgical correction for a patient who was suffering [...] - Reader Question:
Base Laceration Repair Code on Length and Complexity of The Wound
Question: Our oral surgeon recently reviewed a 21-year-old established male patient who had received a laceration [...] - Reader Question:
Choose Maxillary I&D Codes Based on Origin of Abscess
Question: Our oral surgeon recently performed incision and drainage of an abscess of the maxilla on [...]