Ophthalmology and Optometry Coding Alert
Establish A No-Show Policy?
Question: We have never charged for no-shows, but we’re starting to realize we may be losing money due to this. We’re thinking of starting to charge people if they fail to present for their appointments. How do we know what to charge?
Delaware Subscriber
Answer: Every practice must establish its own policy about whether they should charge for missed appointments. Once you do decide to charge patients for no-show visits, the first thing you must do is create a policy that outlines the criteria in detail. If a policy does not exist, your practice would have little support to enforce a consequence if questioned.
While creating your policy, keep in mind all of the criteria that will be helpful to have in place if you need to charge for the no-show visits. There may be situations when missing an appointment isn’t billable (such as if a patient cancels with an acceptable amount of notice prior to the appointment). For example, if the policy states canceling the visit at least 24 hours in advance is required and the patient does, charging a fee for the missed appointment would not be appropriate since enough advance notice was given. Or, in some cases, policies may say scheduled consultations can be billed if no cancellation is received within a certain timeframe.
Note that Medicare does allow practices to charge the patient for no-shows under certain conditions. The first condition is, rules must be clearly stated in an office’s policy that no-shows are charged and under what circumstances. The second condition is that this policy is universal, and all patients are subject to the same rule and charge and no individual, group, or patient type is exempt.
Once you establish the parameters of the policy, have established patients sign the new policy during their next office visit, and have all new patients sign it with the new patient paperwork. Once they sign the no-show policy, you can charge the patients (and not the insurers) when patients violate the policy.
Related Articles
Ophthalmology and Optometry Coding Alert
- ICD-10 Coding:
Look for New Orbital Fracture, Vision Screening Codes Oct. 1
ICD-10 makes over 400 changes effective this fall. When ICD-10 initially went into effect, many [...] - Advance Beneficiary Notices:
Know These 10 ABN Facts Essential to Eye Care Practices
Hint: If you aren’t aware of coverage guidelines, it’s you who pays — not the [...] - Compliance:
Latest OIG Report Shines Light on EHR Issues
Tip: Make sure your software is on the up and up. Health care fraud goes [...] - You Be the Coder:
Go After These After-Hours Codes
Question: A patient called and said she thought she had a detached retina, and we [...] - Reader Question:
Establish A No-Show Policy?
Question: We have never charged for no-shows, but we’re starting to realize we may be losing [...] - Reader Question:
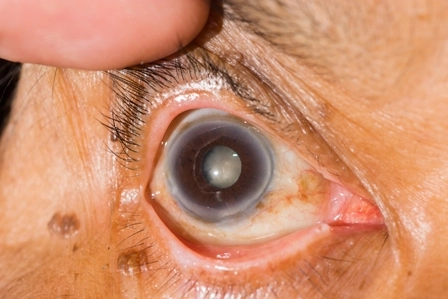
Understand the Corneal Abrasion Dx Codes
Question: A new patient came in with pain, redness, and tearing in her right eye. She [...] - Reader Question:
Check Contracts When Waiving Copays
Question: We have a few patients at our practice who aren’t charged anything when they visit [...] - Reader Question:
Look to G Codes for Glaucoma Screenings
Question: Our ophthalmologist keeps circling E/M codes like 99212 when he performs glaucoma screenings for high-risk [...]