Can You Accurately Diagnose These 3 Infrequently-Seen Eye Conditions?

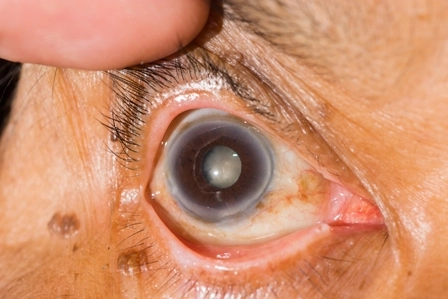
Put the codes for coloboma, Behcet's Disease and more into your toolkit. You may know the asthma and COPD diagnosis codes by heart, but that doesn't mean you're just as much of an ace with diagnoses that your ophthalmologist sees less frequently. Get a handle on how to code these three rare eye disorders with a few quick tips. 1. Not All Colobomas Are Diagnosed at Birth When patients have colobomas, that means they were born without certain tissues that form the eye. These colobomas are frequently seen in the iris because they are more obvious there since it's noticeable when part of the iris is missing. However, colobomas can also affect the other areas that aren't as easy to see on visual examination of the patient, and can be slower to diagnose. When patients present with this condition, they could complain of the following symptoms, among others, which you should report in the absence of a confirmed diagnosis: If the ophthalmologist definitively diagnoses the patient with a coloboma, you'll bill the claim using the more specific code, depending on the location. Several options are listed below: If other conditions are associated with the coloboma, you can report them as well (such as glaucoma or strabismus), but do not report the signs and symptoms if the physician has definitively diagnosed the patient with coloboma. 2. Look to 'M' Codes for Behçet's Disease Ophthalmologists are sometimes called to diagnose and evaluate Behçet's Disease, an inflammatory disorder that causes inflammation throughout the body and can affect patients' eyes so severely that blindness can result. If the ophthalmologist is involved before the Behçet's Disease diagnosis is made, you'll code the symptoms he treats, which can include visual disturbances (H53.8), low vision (H54.5x), blindness (H54.x), ocular pain (H57.1) or eye inflammation, among other signs and symptoms. Once the patient is formally diagnosed with Behçet's Disease, you'll report M35.2 (Behçet's Disease), which »» is located in ICD-10's "Diseases of the Musculoskeletal System and Connective Tissue" section due to the fact that it is an inflammatory disorder. 3. Wait for Confirmation Before Reporting Pigmentary Retinal Dystrophy Patients with pigmentary retinal dystrophy, also referred to as "retinitis pigmentosa," experience vision loss, sometimes just at night or only peripherally. The genetic disorder can be hereditary, but it rarely causes complete blindness. Patients who present with suspected retinitis pigmentosa typically complain of visual disturbances (H53.8), low vision (H54.5x), blindness (H54.x), night blindness (H53.60), peripheral vision loss (H53.459), or other low vision complaints. You should report these signs and symptoms if the definitive diagnosis of pigmentary retinal dystrophy is not yet made. Once the eye care specialist confirms a retinitis pigmentosa diagnosis, you'll report H35.52 (Pigmentary retinal dystrophy), the sole ICD-10 code listed for this condition.