Part 1: Nix 99201 From Your New Patient Office E/M Codes in 2021
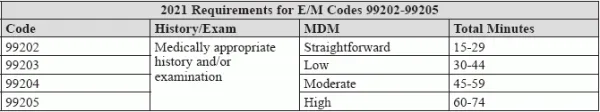
Tip: Look at either MDM or time to choose the appropriate outpatient code. You may not often report 99201 in your oncology practice, but as of right now, the option is available. Come January 1, 2021, this will no longer be the case. Your outpatient claims for new patients are about to drastically change. The lowdown: Not only will you strike 99201 from your potential options, but you’ll need to put a new emphasis on medical decision making (MDM) and time in your oncologist’s documentation. Editor’s Note: This is part one of a series of articles appearing this year in the Oncology Coding Alert, designed to get you ready for this change. Stay tuned for more information. Here’s Why You’ll Say Goodbye to 99201 If you look at the code descriptor for 99201 (Office or other outpatient visit for the evaluation and management of a new patient, which requires these 3 key components: A problem focused history; A problem focused examination; Straightforward medical decision making …), you’ll see it requires “straightforward MDM.” Now review the code descriptor for 99202 (Office or other outpatient visit for the evaluation and management of a new patient, which requires these 3 key components: An expanded problem focused history; An expanded problem focused examination; Straightforward medical decision making…). This also requires “straightforward MDM.” With the new emphasis on MDM for code selection, these two codes are essentially redundant. Check Out Changes to 99202-99205 So the new codes, as of January 1, 2021, won’t require the three components and won’t reference typical face-to-face time. Here’s what they will include. You’ll see the code descriptors describing “a medically appropriate history and/or examination.” Then, your code selection will be based on the MDM level or the total time the oncologist spent with the patient on that date of service. For instance, here is the difference in code descriptors for 99203: All of the outpatient codes for new patients (99202-99205) follow this structure. Notice how this descriptor specifies both a level of MDM and time. The other codes do as well. Here’s a breakdown of these requirements in table form: Keep in mind: If this new outpatient visit lasts more than 74 minutes, you’ll report a prolonged services add-on code temporarily referred to as +99XXX. “You can report 99205 with the prolonged services code when 75 minutes is reached,” says Raemarie Jimenez, CPC, CIC, CPB, CPMA, CPPM, CPC-I, CCS, senior vice president of product at AAPC and coding liaison to the AMA CPT® Editorial Panel. Example: Suppose your oncologist meets a new patient in the office, and the visit consists of a new problem your physician needs to further investigate to determine the necessary course of action. Multiple tests are ordered, including labs, and an ultrasound study. While the physician may suspect an invasive neoplasm, with the condition remaining undiagnosed and no certain prognosis being made, the medical decision making is of moderate level along with the visit lasting 45 minutes. If that’s the case, your physician would report 99204. “You do not need both MDM and time,” Jimenez says. In other words, you could look at either the time in this example (45 minutes) or the level of MDM (moderate level), and this will direct you to 99204. Note: However, this change does not mean providers should skip performing a history and exam, experts say. The provider should obtain a medically relevant history and exam, Jimenez says. Although history and exam will not be factored into choosing the E/M level, they are still an important part of the medical record. It is up to the physician’s clinical determination of what level needs to be performed and documented. Experts agree now is the time to start learning about these upcoming changes. Familiarize yourself with the guidelines and create educational materials for your physicians and coders, says Suzan Hauptman, MPM, CPC, CEMC, CEDC, director compliance audit at Cancer Treatment Centers of America. Teach everyone, now (perhaps with a side-by-side comparison) on what the changes will look like next year. Examples might be a good way to illustrate this best. “Emphasize with all healthcare providers that it is not the amount of documentation, but rather the content,” Hauptman adds. Editor’s Note: Have more questions about how new E/M codes will change in 2021? Email the Oncology Coding Alert editor at suzanneb@codinginstitute.com.