Ob-Gyn Coding Alert
Same-Day Insertion, Removal May Be Subjected to Payer Policies
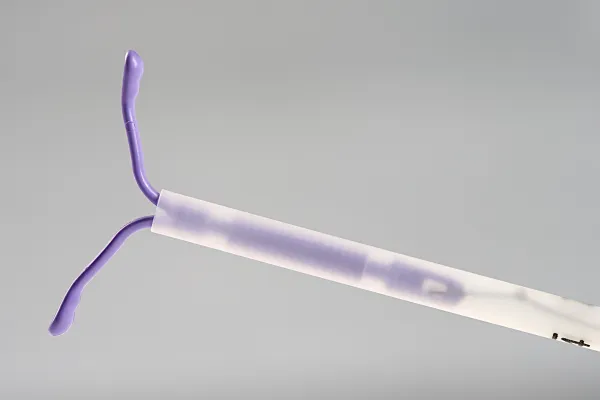
Question: A patient has an intrauterine device (IUD) place in the morning. She returns to the office late in the same day in pain and wants the IUD removed. The ob-gyn removes it. Is this considered two office visits? Do you still bill for the IUD? Any modifier needed? I am stumped. South Carolina Subscriber Answer: Unless your ob-gyn documented a separate and distinct evaluation and management (E/M) service, you should not bill an office visit at all. You should certainly bill for inserting the IUD (58300) and the removal (58301). You provided the services and should be paid for the work of both. As 58300 does not have any global days, these two codes should not be subjected to National Correct Coding Initiative (NCCI) edits, and you should not need a modifier for the removal. Notice the “should not” in that sentence, as some carriers will create their own policies regarding these types of situations. Also, note that the code 58300 is not a Medicare-covered service. For this reason, no NCCI edits were created with this code.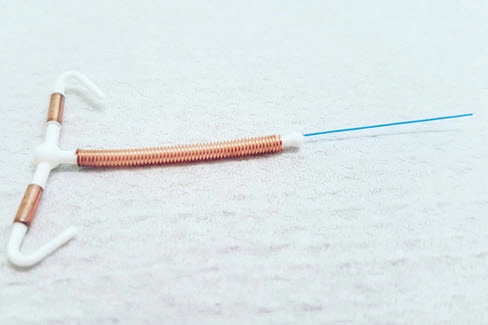
Related Articles
Ob-Gyn Coding Alert
- Obstetrics:
Do You Know the Difference Between Reporting 59000 or 59001? Find Out.
Here’s why you should look for the term “polyhydramnios.” You may think you’re an amniocentesis [...] - Gynecology:
Pinpoint the Perfect Pessary Code With This Expert Advice
Refitting plus insertion may mean you can report more than an E/M service. Although you [...] - ICD-10-CM:
“Aftercare,” “Monitoring,” and “Surveillance” Are not Interchangeable
Never, ever report aftercare and monitoring codes together. When you’re applying ICD-10-CM codes for ongoing [...] - You Be the Coder:
Repeat Pap Plus UTI
Question: A high-risk Medicare patient came in for her annual wellness visit. The ob-gyn did a [...] - Reader Questions:
Help Your HIPAA Compliance Achieve Perfection
Question: At our practice, we take HIPAA compliance very seriously. In fact, we regularly utilize risk [...] - Reader Questions:
Determine What Diagnoses Can Be Principal Ones
Question: Our auditors have given us a list of unacceptable principal diagnosis codes. They want us [...] - Reader Questions:
Same-Day Insertion, Removal May Be Subjected to Payer Policies
Question: A patient has an intrauterine device (IUD) place in the morning. She returns to the [...] - Reader Questions:
Confidently Report Counseling Codes in Conjunction with E/M
Question: Can an ob-gyn bill for alcohol abuse and intervention in addition to an E/M visit? [...]