Ob-Gyn Coding Alert
Coding Quiz:
Are You an Expert When It Comes to Modifier 25 Versus 57? Find Out
Published on Wed Sep 05, 2018

You’ve reached your limit of free articles. Already a subscriber? Log in.
Not a subscriber? Subscribe today to continue reading this article. Plus, you’ll get:
- Simple explanations of current healthcare regulations and payer programs
- Real-world reporting scenarios solved by our expert coders
- Industry news, such as MAC and RAC activities, the OIG Work Plan, and CERT reports
- Instant access to every article ever published in Revenue Cycle Insider
- 6 annual AAPC-approved CEUs
- The latest updates for CPT®, ICD-10-CM, HCPCS Level II, NCCI edits, modifiers, compliance, technology, practice management, and more
Related Articles
Other Articles in this issue of
Ob-Gyn Coding Alert
- ICD-10 Update:
Thwart Potential Claim Disasters By Underlining 2 Ob-Gyn Guideline Revisions
Hint: Avoid reporting BMI diagnoses during pregnancy. You learned the new ICD-10-CM codes premiering October [...] - Obstetrics:
Bust 4 Myths to Conquer Contraceptive Service Coding
Find out whether preventive services include counseling. Do you know when you should code a [...] - Gynecology:
How to Untangle Your Nonsurgical SUI Treatment Coding Options
Here’s how to report training involving biofeedback. Before turning to surgical treatments for stress urinary [...] - Coding Quiz:
Are You an Expert When It Comes to Modifier 25 Versus 57? Find Out
Scheduling a surgery for next week may not require a modifier at all. If you [...] - You Be the Coder:
Your Lesion Code Depends on Diameter
Question: Our physician performedan excision of 4 benign lesions and wants to bill 11420, but [...] - Reader Question:
Patient Death Doesn't Mean HIPAA Agreement Dies, Too
Question: What does HIPAA say about maintaining patients’ private health information after they die? California [...] - Reader Question:
This is How to Clear Up Your Injection Coding Mistakes
Question: Our ob-gyn injected Depo-Medrol and Xylocaine-into the area of the vaginal cuff that was [...] - Reader Question:
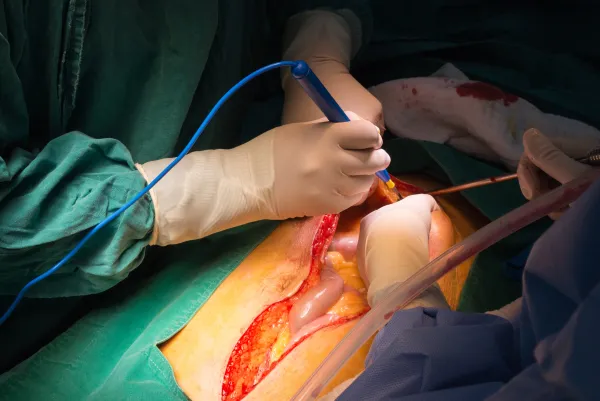
Coding 58925, 49320 Means Specifying Incorrect Surgical Method
Question: My ob-gyn performed a diagnostic laparoscopy with ovarian cystectomy. Would it be wrong to [...] - Reader Question:
Find Out if You Can Report Admin Code With This J Code
Question: What code should I bill for Progesterone 200mg? Can you bill for the administration? [...] - Reader Question:
Update Your Modifiers for Telehealth
Question: If we provide telehealth services from our practice’s offices, do we need to append [...] - Reader Question:
Avoid Protected Health Information Exposure
Question: Do you have any advice to help us protect our patients’ health information, if [...] - Reader Question:
Find Out How Long After Delivery You Can Apply Postpartum Condition
Question: Patient had hysteroscopy with lysis of adhesions and a dilation and curettage (D&C). Diagnoses [...]
View All