OASIS Alert
Will Your M1024 Answers Pass Muster?
Fracture codes are the only acceptable M1024 diagnoses this year.
The home health PPS revisions for 2013 change almost everything about M1024 -- Payment diagnoses. Do you know which codes to list in M1024 and which you shouldn’t?
Old way: Prior to Jan. 1, you were able to list a numerical ICD-9 code in M1024 to earn potential case mix points in three circumstances. These included instances when you listed a V code in M1020 or M1022 that:
- Indicated aftercare for an acute fracture;
- Described care resulting from a resolved condition; or
- Displaced a case mix diagnosis from the Diabetes, Skin 1, or Neuro 1 case mix categories.
New way: As of Jan. 1, under the 2013 Home Health Prospective Payment System, M1024 is reserved for reporting acute fracture codes only.
The good news is, "it’s going to get a lot easier," says Mary Deakle, HCS-D, COS-C, manager of compliance and education with Daymarck Home Healthcare Coding in Bismarck, N.D. "If it’s not a fracture, it doesn’t go there [in M1024]."
But the bad news could be a negative impact on your agency’s bottom line. While the Centers for Medicare & Medicaid Services maintain that this change will have a minimal impact on payment, other experts predict that with almost 60 percent of OASIS assessments including resolved case mix diagnoses in M1024 there will be a noticeable reduction in reimbursement.
Keep Sequencing Straight with Diabetes, Skin 1, Neuro 1
As of January 1, you will no longer list codes from the Diabetes, Skin 1, or Neuro 1 case mix categories in M1024 when they are displaced by a V code in M1020a. These three case mix groups earn higher points when they are listed as primary diagnoses, and listing them in M1024 ensured this reimbursement rate. But now, CMS says they will earn the higher points when they are listed immediately following the V code in M1020a.
For example: Your patient was admitted for aftercare following surgery to remove a benign neoplasm of the brain. Radiation therapy is planned. Prior to Jan. 1, you would have coded as follows, says Judy Adams, RN, BSN, HCS-D, HCS-O, with Adams Home Care Consulting in Chapel Hill, N.C.
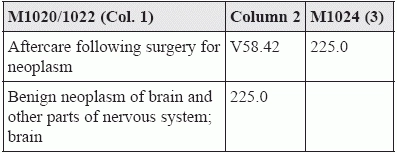
After Jan. 1, you would leave M1024 blank for this patient, Adams says. The sequencing of the codes in M1020/M1022 will remain the same, but making sure that the Neuro 1 code 225.0 immediately follows the corresponding V code is essential in securing the available case mix points.
Questions remain: While CMS says appropriate case mix points will be awarded for Diabetes, Skin 1, or Neuro 1 codes listed immediately following appropriate V codes in M1020a, exactly how that will happen remains to be seen.
"How will the altered grouper to count points correctly?" wonders Deakle. "For example, suppose your patient has a chronic ulcer on his toe with no etiology." He has his toe amputated. The ulcer is gone and you’re providing aftercare. But the patient also has problems with his diabetes that you will be providing care for, so you list the diabetes in M1022b. "How will CMS know whether the diabetes should earn primary points rather than secondary diagnosis points?" she asks.
Take a Closer Look at Resolved Conditions
Homecare agencies will lose the points they once earned for care directed at resolved conditions following surgery, says Lisa Woolery, RN, BSN, BCHH-C, assistant director of clinical coding services with Northampton, MA-based Fazzi Associates.
For example: Suppose your patient had surgery to remove her gallbladder to treat cholecystitis. She is being admitted to home care for aftercare. Prior to Jan. 1, you would report V58.75 (Aftercare following surgery of the teeth, oral cavity and digestive system, NEC) in M1020a and a code for the cholecystitis from the 575.x (Other disorders of gallbladder) category on M1024, allowing you to earn case mix points for the resolved condition.
In this scenario, your patient doesn’t have cholecystitis anymore, because her gallbladder has been removed, so you can’t code for it in M1020 or M1022. But you were able to list the 575.x code in M1024 for case mix points and risk adjustment.
After Jan. 1, however, you would still report V58.75 in M1020a, but you can no longer include a code for your patient’s cholecystitis because it is a resolved condition. And as a result, you will no longer earn case mix points for this diagnosis.
Silver lining? However, while you can no longer earn points for these resolved conditions, such patients often have other conditions for which you can earn points, Deakle says.
For example: "Many of the patients I see that have GI conditions such as cholecystitis sometimes will have other GI conditions such as GERD or stomach ulcers for example," Deakle says. "If the documentation supports coding GERD then you can recapture GI points that would be lost by not being able to use the cholecystitis as it is resolved by surgery."
Coding scenario: Your patient was admitted to home health following a cholecystectomy for cholecystitis. Skilled nursing will provide dressing changes. The patient’s medical history includes type II diabetes, GERD (with new Nexium prescribed), and hypertension. After Jan 1. You would code for him as follows, Deakle says:
- M1020a: V58.75;
- M1022b: 530.81 (Esophogeal reflux);
- M1022c: 250.00 (Diabetes mellitus without mention of complication; type II or unspecified type, not stated as uncontrolled);
- M1022d: 401.9 (Essential hypertension; unspecified); and
- M1022e: V58.31 (Encounter for change or removal of surgical wound dressings).
Because of the 2013 PPS revisions, you can’t list a 575.x code in M1024 opposite the aftercare code for this patient, Deakle says. As a result you lose the GI case mix points for the resolved cholecystitis diagnosis. But because this patient also has a GERD diagnosis with new medication prescribed, you’ll pick up the GI points in M1022 instead.
OASIS Alert
- Item Focus:
M1308: Don't Miss the Points for Pressure Ulcers
There’s no need to report Stage I or closed Stage II pressure ulcers for this [...] - Education:
Avoid These Common ADL Item Errors
Could your ADL item response send a patient to the nursing home? The OASIS ADL/IADL [...] - Tool:
Try This Approach to Assessing Ability
Adjust your phrasing for more accurate answers. When it comes to completing OASIS items, there [...] - Assessment:
Follow These Tips for Better ADL Assessment
Do you have an accurate understanding of all that’s involved in toilet transfer? When completing [...] - PPS 2013:
Will Your M1024 Answers Pass Muster?
Fracture codes are the only acceptable M1024 diagnoses this year. The home health PPS revisions [...] - Diagnosis Coding:
Take 3 Steps with Coding for Infected Surgical Wounds
Must you always report a causative organism code? When coding for an infected surgical wound [...] - 2 Tips Help You Prevent Case Mix Loss
Don’t let this assumption do a number on your reimbursement. While you can no longer [...] - ICD-10 Update:
ICD-10: Seven Digit ICD-10 Codes Mirror ICD-9 for Infected Surgical Wounds
Remember to list an additional code to describe the infection. The codes you report for [...] - Industry Notes:
Take Advantage of New OASIS Training Resource CMS has posted a new OASIS web based [...]

