OASIS Alert
M1350: Don't Let Your Patients' Wounds Fall through the Cracks
Here’s your chance to secure risk adjustment for wounds.
You can earn case mix points through your answers to many of the OASIS wound items, although not all wounds are eligible for them. Make sure you don’t overlook this essential wound item just because it doesn’t earn points.
Key: OASIS item M1350 — Does this patient have a Skin Lesion or Open Wound can impact an episode’s risk adjustment and is the only place where you can get credit for caring for a wide variety of wounds not covered by other OASIS wound items.
In detail, OASIS item M1350 asks "Does this patient have a Skin Lesion or Open Wound, excluding bowel ostomy, other than those described above that is receiving intervention by the home health agency?" In other words, M1350 asks you whether your agency is providing care for a wound not reported in the other OASIS wound items.
Answering M1350 accurately is especially important because it can identify a discrepancy between the diagnosis codes you list in M1020/M1022 and your OASIS answers, says Ann Rambusch, MSN, HCS-D, HCS-O, COS-C, RN, with Rambusch3 Consulting in Georgetown, Texas. Make certain you’re answering this item correctly to avoid drawing undue scrutiny.
For example: Your OASIS could earn a closer look when you have a diabetic ulcer coded in M1020 and M1022 but M1350 is answered "No."
Know Which Wounds Qualify for M1350
You’ll report wounds like pressure ulcers and surgical wounds elsewhere on the OASIS. But M1350 gives you an opportunity to report conditions like rashes, lesions, and skin tears. Diabetic ulcers and arterial ulcers as well as traumatic wounds are among the common types of wounds you can report in M1350
Definition: A lesion is "a broad term used to describe an area of pathologically altered tissue," according the OASIS item-specific guidance.
Caution: Your agency must be providing care to these lesions in order to answer "1 — Yes," Rambusch points out. For example, if you’re observing a rash, or providing care for lower extremity edema you can safely report the wound in this item.
Refer to the following table when answering M1350 for help in determining whether your patient’s wound qualifies for inclusion:
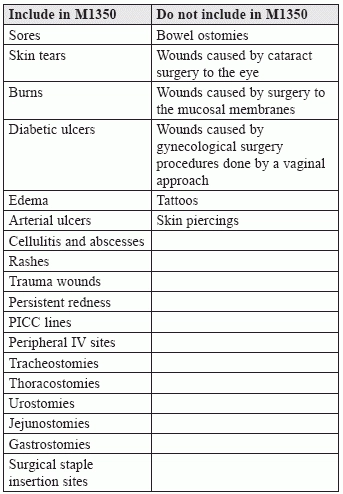
Note: Don’t report tattoos, piercings, or other skin alterations in M1350 unless you are providing ongoing assessment or clinical intervention for them, CMS advises.
You have a good amount of leeway in considering whether to report a skin lesion in M1350. "Many different types of skin lesions exist," CMS says in the newly updated annual collection of OASIS Q&As. "These may be classified as primary lesions (arising from previously normal skin), such as vesicles, pustules, wheals, or as secondary lesions (resulting from changes in primary lesions), such as crusts, ulcers, or scars. Other classifications describe lesions as changes in color or texture (e.g., maceration, scale, lichenification), changes in shape of the skin surface (e.g., cyst, nodule, edema), breaks in skin surfaces (e.g., abrasion, excoriation, fissure, incision), or vascular lesions (e.g., petechiae, ecchymosis)."
But, "for the purposes of scoring M1350 you will only report [these lesions] if the patient has a skin lesion or open wound that is receiving intervention by your agency," CMS reminds.
Establish the Basics
Your response options for M1350 are simple:
0 — No or
1 — Yes.
Caution: Before you select response "1," make certain that documentation also indicates that you are providing care for this patient’s skin lesion or wound. But don’t hesitate to count the wounds and lesions you are caring for here.
Nurses often don’t think about taking credit for care of conditions like edema or rashes, Rambusch says. But when you are watching or caring for these wounds, M1350 is your opportunity to take credit.
Tip: If you’re observing a wound, like a rash, you should have at least one intervention on the plan of care, Rambusch says. For example: "Observe and report if rash worsens."
But don’t hold yourself to an overly restrictive standard for this item, says Karen Vance, OTR, supervising consultant with BKD in Colorado Springs, Colo. Do you really need to have a separate line item and separate section for the patient’s wound care? Or can you include it with other care such as teaching about a healthy diet to promote wound healing?
Tip: The intervention doesn’t need to be provided on the day of the assessment; your agency just needs to be providing ongoing assessment and/or clinical intervention as part of the planned or provided care.
Bottom line: If your patient has any skin condition that qualifies for inclusion in M1350 and you are clinically assessing the lesion on an ongoing basis as indicated on the plan of care, you can answer "1 — Yes" for this item.
Why M1350 is Important
Clinicians often think M1350 doesn’t matter because it doesn’t earn points, Rambusch says. But "we spend a lot of time working with edema, burns, and traumatic wounds. We want to be receiving credit for these in M1350," she says
Plus: When you miss listing these lesions and wounds in M1350 but you have listed diagnosis codes for them in M1020/M1022, you may be telling reviewers that you don’t know what you’re talking about, Rambusch says.
So if you’re coding for a diabetic ulcer, an arterial ulcer, an abscess or cellulitis in M1020/M1022, make sure to check that you answer M1350 "1 — Yes," Rambusch reminds "Check that ‘not only did I code it, but did I give myself credit?’ she says."
Impact: Prior to the current nonroutine supplies payment system, home health agencies didn’t bill for a lot of wound supplies, Rambusch points out. But CMS used the data from those agencies that did bill to craft the current NRS payment system. "We never know when data we report — or don’t report — will come back to haunt us," she says.
And while you won’t earn case mix points for M1350, the data reported here is used in risk adjustment, so you’ll miss out if you answer this item incorrectly, Rambusch says.
"This item shows another facet of the patient’s condition that requires care. "Make sure you’re giving yourself credit," Rambusch says.
For example: Suppose you’re providing care including Pleurx catheter changes for a patient with a thoracostomy. Thoracostomies are not surgical wounds, Rambusch says. "There are 10 Pleurx catheters in a box, which runs about $700. You usually need at least one box for a patient," she says.
With this patient, you get no credit for a surgical wound and no NRS payment, Rambusch says. "You should at least get risk adjustment. These patients have skin lesions and you are providing care."
OASIS Alert
- Item Focus:
M1350: Don't Let Your Patients' Wounds Fall through the Cracks
Here’s your chance to secure risk adjustment for wounds. You can earn case mix points [...] - OASIS Conventions:
Know the Time Frame for Each Item
Do you know what counts as ‘recent past’? Knowing which time period to consider for [...] - Tools:
Is This Fall Risk Tool Appropriate for Your Agency?
Ask the right questions before making a change. Home health agencies struggling with answering M1910 [...] - HIPAA Compliance:
3 Tips to Safeguard Patient Data On Mobile Devices
Prevent unauthorized access or risk big fines. Recent breaches underline the importance of keeping electronic [...] - Education:
These Expert Tips will Ease Your ICD 10-CM Transition
There’s no time like the present to get your ICD-10 plans underway. Taking the time [...] - ICD-10 Update:
Check Your ICD-10 Readiness
Don’t jump in head first with coding preparation. Next year’s transition to ICD-10 will impact [...] - ICD-10 Preparation:
Get to Know These ICD-10 Conventions
Not everything changes in ICD-10. While it’s too early to worry over all the intricate [...] - Industry Notes:
Does Your Fall Risk Assessment Cover These Bases?
Don’t overlook environmental risks. Falls are the leading cause of fatal injury among older adults [...] - Reader Question:
When Coding Logic and M1350 Conflict
Question: Our patient was hit by a metal swing and suffered a deep laceration to [...]

