OASIS Alert
M1100: Make the Right Choice for Every Patient in 2 Steps
These key elements determine your patient’s living arrangement and available assistance.
Reporting with whom your patient lives and when they can provide assistance may not seem all that difficult, but if you mark the wrong OASIS response to M1100, your agency’s outcomes could suffer. Break this item into two parts and you’ll have a better grasp on how to answer accurately.
OASIS item M1100 — Patient Living Situation uses a chart (see below) to help clinicians determine whether a patient lives alone and if there are people living with him who can provide physical assistance. But navigating this chart isn’t always straightforward — you need to know some background before you can select the right response.
Answer Based on Usual Arrangement
Common pitfall: It’s important to make sure you base your response to this item on your patient’s usual living arrangement, says Judy Adams, RN, BSN, HCS-D, HCS-O, with Adams Home Care Consulting in Asheville, N.C. Your answer should reflect what is generally the situation for this patient, not a temporary change in living situation due to her condition — unless the new living situation is expected to be permanent.
For example: Suppose your patient normally lives alone with only occasional short-term assistance. She has her daughter living with her while she recovers from surgery. At the current time, the daughter is available all the time. You might be tempted to select response “06 — Patient lives with other person(s) in the home; around the clock.” But if this arrangement is a temporary one and not expected to be a permanent change, you should answer “04 — Patient lives alone; occasional short-term assistance,” Adams says.
Break this Question Down
This question is best answered with a two-step approach, Adams says. First, assess the living situation, and then look at the amount of assistance the patient receives on a regular basis.
1) Determine where and with whom the patient lives. The first step to selecting your M1100 response is to find out whether your patient lives alone, with another person in the home, or in a congregate situation, Adams says.
Lives alone: To report a patient as “living alone,” he must be living in an independent (non-assisted) setting, Adams says. This could be a home, apartment, or in his own room in a boarding house. A patient also qualifies as “living alone” when he normally lives alone but has a temporary caregiver living in the home to provide assistance or when he has only paid live-in help, she says.
With others: When any other people also call the patient’s house “home,” you’ll select a response from Row B. That can mean the patient lives with a relative, friend, or non-related housemate.
Tricky: When answering M1100, you’ll select “with others” if your patient lives with family members paid to care for her, but you’ll choose “lives alone” when the patient has unrelated paid live-in help.
Congregate: Any living situation where the patient receives supervision or oversight as part of the arrangement counts as an assisted or congregate setting, the Centers for Medicare & Medicaid Services states in the OASIS-C Guidance Manual, Chapter 3. This includes assisted living communities, residential home care, and personal home care.
Tip: Provide a living arrangement “cheat sheet” to clinicians to help improve accuracy with this step, says Annette Lee, RN, MS, HCS-D, COS-C, AHIMA ICD-10 Trainer with Redmond, Wash.-based OASIS Answers. Break down the rows for this item and include the following definitions and information:
2) Determine how much assistance is available. This can be a challenge.
The first thing to keep in mind when considering when your patient has assistance is that all the assistance you report in this item must be actual in-person help, Adams says. For a patient who lives alone or with others, don’t count emergency help by phone, or an emergency response system that can signal for assistance if needed. But for those in a congregate setting, a call-bell that can summon help does count as in-person assistance.
Assistance can be from people living outside the home or from a number of different people, Adams points out. Base the amount of assistance on the availability of regular assistance. Your response should depend on the consistency of available assistance, not limited to one person.
For example: Your patient’s children take turns staying with her from supper time through the night each night. There is someone there to assist her each night, although it may not be the same person every night. You would score this patient as “3 — Patient lives alone; regular nighttime assistance” even though it is a different person who is there each night, Adams says.
Use Your Judgment
You’ll need to use your clinical judgment to determine which hours constitute regular nighttime or regular daytime based on the patient’s specific activities and routines, Adams says. The OASIS-C Guidance Manual doesn’t designate any particular hours as “regular daytime” or “regular nighttime.”
You’ll also need to consider the expected ability of the person to be able to provide assistance.
For example: Your patient lives with another relative in the home, but that relative is unable or unwilling to provide needed assistance. You’ll choose response “10 — Lives with another person, no assistance available,” for this patient, Adams says.
Resources: For examples of patient situations and appropriate scoring, download Chapter 3 of the OASIS-C Guidance Manual at www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HomeHealthQualityInits/HHQIOASISUserManual.html.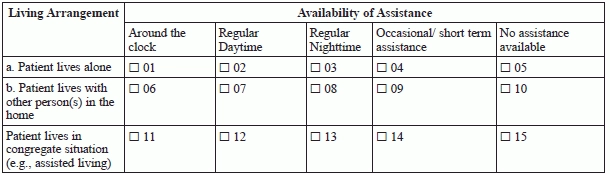
OASIS Alert
- Item Focus:
M1100: Make the Right Choice for Every Patient in 2 Steps
These key elements determine your patient’s living arrangement and available assistance. Reporting with whom your [...] - Try Your Hand at this M1100 Scenario
Consider availability of assistance in the home. Think you’ve got answering M1100 — Patient Living [...] - OASIS Conventions:
Understand Episode Definitions or Expect an Outcomes Ding
Not all episodes are created equal. Among the 16 general conventions for completing an OASIS [...] - Documentation:
Master 7 Qualities for Top Notch Documentation
Make sure you’re supporting medical necessity and code selection or risk denials. You already know [...] - Quiz:
Test Your Cognitive Functioning Skills
Confusion and cognitive functioning answers don’t always need to match up. When it comes to [...] - Clip and Save:
Boost Your Cognitive Functioning Accuracy with this Tool
Know when and where to report confusion. When assessing a client’s cognitive status, including behaviors [...] - ICD-10 Diagnosis Coding:
Look to the Alphabetic Index for an ICD-10 Diabetes Jump Start
Watch for more types of diabetes. Most likely, you can practically code for diabetes in [...] - ICD-10 Diagnosis Coding:
9 Steps Guide the Way to a Successful ICD-10 Transition
Is your documentation up to ICD-10 standards? You may feel like you’re running just to [...] - Industry Notes
Buckle Down On Rehospitalization Efforts. Reducing rehospitalization rates among your patients is good for them, [...]

