See How OASIS and Coding Intersect with Neuro 1 Diagnoses
Don’t let poor documentation derail your reimbursement .
The Neuro 1 case mix category allows you to earn case mix points for patients with a wide range of brain disorders and paralysis To make sure you’re getting all the credit you deserve for treating these patients, make sure your OASIS responses and diagnosis coding are in synch.
The Neuro 1 codes make up one of only three case mix categories that earn different case mix points when listed as a primary diagnosis versus listed as a secondary diagnosis, says Judy Adams, RN, BSN, HCS-D, HCS-O, with Adams Home Care Consulting in Chapel Hill, N.C.
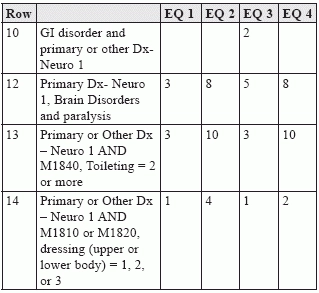
The table below outlines the points available for Neuro 1 diagnoses.
Table 4: Case Mix Adjustment Variables and Scores for Neuro 1 Codes
Synergy Delivers Points
Row 12 in the table above shows that you can earn three to eight points when your patient’s primary diagnosis falls in the Neuro 1 category. But the other opportunities for earning Neuro 1 case mix points aren’t quite so cut and dry.
There are no points available for simply including a Neuro 1 diagnosis as a secondary code, but there are several situations where you can earn additional case mix points from the combination of a Neuro 1 diagnosis and certain functional limitations reported elsewhere on the OASIS, Adams points out.
You’re eligible for additional case mix points when your patient has a Neuro 1 diagnosis and:
A GI disorder diagnosis listed in M1020/M1022 ;
A score of 2 or more for M1840 — Toilet Transferring; or
A score of 1, 2, or 3 for M1810 — Current ability to dress upper body safely or M1820 — Current ability to dress lower body safely.
And if your patient qualifies for case mix points under both rows 13 and 14, you’ll earn points for both.
Score Based on Need for Assistance
A score of 2 or more for M1840 means that your patient is unable to use the toilet safely and has to use a bedside commode, bedpan/urinal or is completely dependent in toileting in order to be safe, says Lisa Selman-Holman, JD, BSN, RN, HCS-D, COS-C, HCS-O, consultant and principal of Selman-Holman & Associates and CoDR — Coding Done Right in Denton, TX. A score of 1, 2, or 3 for M1810 means the patient needs assistance to dress in order to be safe, even if it’s just to set out the clothes for the patient.
Tip: The additional case mix points available when OASIS functional items and Neuro 1 diagnosis coding interact are also available when the Neuro 1 code is the primary diagnosis
Coding scenario: Your patient was hospitalized for surgery to remove a glioblastoma multiforme (malignant brain tumor) of the brain stem. During the surgery, the patient had an intracranial hemorrhage that resulted in a cerebrovascular accident (CVA) with residual hemiplegia of the dominant side. Treatment continues for the malignant tumor, but the home health primary focus of care is on the dominant sided hemiplegia. Your agency will be providing physical therapy, occupational therapy, and skilled nursing when he returns home. Code for this patient as follows, Adams says:
M1010 (Inpatient Diagnosis) and M1016 (Diagnoses Requiring Medical or Treatment Regimen Change within Past 14 Days):
997.02 (Iatrogenic cerebrovascular infarction or hemorrhage);
432.9 (Unspecified intracranial hemorrhage); and
191.7 (Malignant neoplasm of brain stem).
M1020a: 438.21 (Late effect of cerebrovascular disease, hemiplegia affecting dominant side);
M1022b: V58.42 (Aftercare following surgery for neoplasm); and
M1022c: 191.7 (Malignant neoplasm of brain stem)
Explanation: You can report your patient’s CVA in M1010 and M1016. You’ll see a note under 997.02 indicating that you should list an additional code to specify the type of postoperative stroke involved. In this case, that code is 432.9. Because the patient’s surgery addressed his brain tumor, you should also list 191.7 here.
While you can list an iatrogenic CVA in both M1010 and M1016, the code is restricted to the hospital. So once the patient reaches home health, your coding changes to the late effect code for any residuals, Adams says.
Your patient’s hemiplegia is the primary reason he requires home care. In this case, the hemiplegia is a late effect of a CVA, so you’ll list late effect code 438.21 in M1020a.
It’s appropriate to list an aftercare for surgery code. In this case, V58.42 is your code because the surgery was performed to remove his brain tumor.
Your patient will require routine aftercare following the surgery for neoplasm, but also observation and assessment of the effects of the malignancy since it is still being treated, Adams says. For these reasons, you can list Neuro 1 code 191.7 as an additional current diagnosis.
Because 191.7 isn’t your primary diagnosis, you won’t earn any case mix points for your patient’s malignant neoplasm alone, even though it is a Neuro 1 code.
If the patient requires assistance with either toileting or upper or lower body dressing, and this is properly documented on the OASIS in M1840, M1810, or M1820, you will be eligible for Neuro 1 case mix points from rows 13 and 14.
A patient with late effect hemiplegia of the dominant side who still requires treatment for a brain tumor is likely to have functional problems with dressing or toileting, allowing you to earn points in those areas, Adams says. If the patient has deficits in both dressing and toileting, you could earn as many as 14 points.
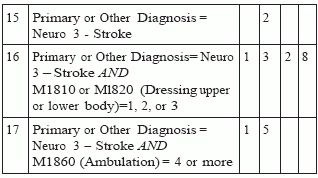
In addition, the hemiplegia will earn Neuro 3 points (see table below).
Table 4: Case Mix Adjustment Variables and Scores for Neuro 3 Codes
An ambulation score of 4 or more means that the patient is unable to ambulate safely even with assistance and a device, Selman-Holman says.