Neurology & Pain Management Coding Alert
Study This Case to Prep for New Year
Deciding cases by MDM will be a top challenge in 2021. We’ve all been prepping for the past year for what’s coming next month: the new guidelines and descriptors for office/outpatient evaluation and management (E/M) services. Now it’s almost time for action. Are you ready? Keep calm, and code on: The new E/M rules haven’t changed since we they were finalized; trust what you’ve learned and go into the new year armed with confidence. Here’s one last try at coding a complicated scenario with the 2021 E/M rules, courtesy of Jaci Johnson Kipreos CPC, CPMA, CDEO, CEMC, COC, CPC-I, president at Practice Integrity, LLC in San Diego. Kipreos presented this case, along with several others, during the AAPC webinar “2021 E/M Guideline Changes: Neurology.” Use This Chart Since coding based on encounter time is very straightforward, we’re going to focus on the other method by which you’ll be able to choose an office/outpatient E/M code in 2021: medical decision making (MDM). Here’s the MDM chart for each office/outpatient E/M code starting in 2021: 2021 Office/Outpatient Coding Based on MDM The Case Initial Office Visit Note Date: 03/19/XX CHIEF COMPLAINT: breakthrough seizures HPI 4-year-old male presents for seizures. Taking 2.5 mls Keppra BID. Continues to have breakthrough seizures during sleep with shaking of arms and or legs. Otherwise tolerating medication with no additional side effects. No recent ER visit/ illness. Denies: headaches, vision changes, weakness, gait instability. Analysis: “I know that the patient is on medication. So, when I get to the assessment is there going to be any change in medication?” Kipreos asked. “I’m starting to get a sense of complexity. He’s having breakthrough seizures and the medication is not really covering it. Now, what I find interesting, we have a 4-year-old patient, we have history — but I don’t know who provided it. So as of now, I cannot give credit for an independent historian because I don’t know who it is.” PAST MEDICAL HISTORY • Heart murmur • Seizures PAST SURGICAL HISTORY History reviewed. No pertinent surgical history. SOCIAL HISTORY Attends daycare 4 days a week. No exposure to 2nd hand smoke. MEDICINES Current Outpatient Prescriptions: • diazepam (DIASTAT) 2.5 mg Kit rectal kit, Place 5 mg rectally, Disp: Rfl: • levetiracetam (KEPPRA) 100 mg/mL oral solution, Take 2.5 mL by mouth 2 (two) times daily, Disp: Rfl Analysis: “Here we see appropriate information. I’m looking at it to see if there is something here that could add to the complexity,” Kipreos explained. REVIEW OF SYSTEMS See HPI All other systems reviewed and are negative. PHYSICAL EXAM Weight Readings 03/19/1914.3 kg (4 %, Z= -1.70)* BMI 15.5 kg/(m^2). Constitutional: He is active. Mouth/Throat: Mucous membranes moist. Eyes: Pupils equal, round, and reactive to light. Conjunctivae and EOM are normal. Neck: Normal ROM. Cardiovascular: Normal rate and regular rhythm. Pulmonary/Chest: Effort normal, breath sounds normal. Abdominal: Full and soft. Bowel sounds normal. Musculoskeletal: Normal ROM. Neurological: He is alert. Skin: Skin warm and moist. Analysis: “The review of systems [ROS] is appropriate,” said Kipreos. LABS Labs -OAs, AAs serum and urine, lactic acid, pyruvate -normal-----CSF studies negative for HSV/infection Ammonia elevated, no evidence of encephalopathy IMAGING Renal US 1/15/2015 –normal MRI brain w/& w/o contrast 1/14/2015 -subependymal nodules w/gray matter signal characteristics along the lateral ventricles, right greater than left (primary consideration is for tuberous sclerosis); increasing size of the ventricular system which is concerning for developing hydrocephalus CT head 9/19/2014 –normal MRI brain 1/8/2019 -cortical tubers and subependymal nodules c/w TS OTHER TESTS ECHO 1/15/2015 -history of tuberous sclerosis; thickened and domed pulmonary valve w/ mild annular hypoplasia and mild valvar PS, Vmax 2.5m/sec; o/w anatomy of heart normal EEG 2/18/2015 -normal EKG 8/7/2017 –normal EEG 1/8/2019 -normal (sedated) Analysis: “We have various labs noted and they’re all normal, and we have mention of the ammonia elevation,” Kipreos explained. “Again, this is a new patient for this provider, so I know they have not ordered these labs. I can see that they reviewed the results, because they made notes.” “Imaging has also been reviewed. Per date of service, I can tell that some of this imaging is older; however, it’s all new to this provider, so they get credit for reviewing all of this info,” continued Kipreos. Kipreos saw no evidence of individual independent interpretation of any of these tests. “This provider is providing information based on what they read and making the statement that everything was reviewed and they have that information,” she stressed. ASSESSMENT & PLAN: 1. Localization-related (focal) (partial) symptomatic epilepsy and epileptic syndromes with complex partial seizures, intractable, without status epilepticus Increase Keppra to 3.5 mls BID, approx. 48 mg/kg/day) to see if benefit. Notified to RTC or call for any additional increase in seizure. Keppra level last visit in January 2019 was normal. Labs next visit. Re-educ seizure precaution and first aid. Analysis: “We know that the patient is still having breakthrough seizures, which gives me an indication of the complexity. The provider is also making an increase in the medication,” Kipreos said. However, the “Labs next visit” note is unclear. “First, I don’t know what labs they are. Second, I don’t know if this is checking for toxicity. “If I wanted to infer these things, it’s not possible. I would need clear information” to give credit for labs ordered, Kipreos said. Remember: “Even if I happen to work in this office, and I know the standard labs always ordered, it doesn’t matter. It has to be documented somewhere in the record,” she continued. MDM Components Number and Complexity of Problems Addressed: Moderate Kipreos pegged this as a chronic condition with an exacerbation. “The patient is having breakthrough seizures, they’re on medication that’s not doing everything it should be doing for the patient. So, we’re comfortable with Number and Complexity of Problems Addressed as moderate,” she explained. Amount and/or Complexity of Data to be Reviewed and Analyzed: Moderate “We had a lot of data with this patient. There were definitely over three unique tests reviewed, which would satisfy Category 1,” explained Kipreos. “For moderate data, we need it to satisfy one of the three categories. And Category 1 is asking for at least three data points, which we do have. That’s all in the tests reviewed. It’s a comfortable, solid moderate level.” Risk of Complications and/or Morbidity or Mortality of Patient Management: Moderate “Because of prescription management, it is moderate risk. The patient came in with a prescription already; but this provider is going to manage it and increase it, and therefore we’re going to give them credit for that thinking and the risk associated,” Kipreos concluded. Coding Based on MDM, you’ll code this encounter as 99204 (Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and moderate level of medical decision making. When using time for code selection, 45-59 minutes of total time is spent on the date of the encounter. …) in 2021. (This descriptor for 99204 is to take effect January 1, 2021.)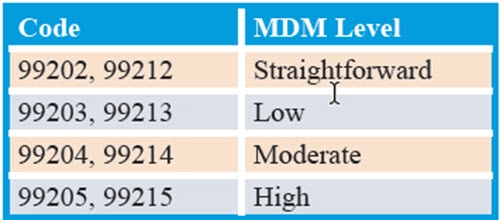


Neurology & Pain Management Coding Alert
- 2021 E/M Changes:
Study This Case to Prep for New Year
Deciding cases by MDM will be a top challenge in 2021. We’ve all been prepping [...] - ICD-10 Coding:
Back to Basics: This Guide Resolves Back Pain Dx Problems
… plus, here’s 3 scenarios to help you navigate the M54.- codes. Do you feel [...] - Injection Intro:
Use These Tips to Get Protection on Injection Claims
Here’s why ICD-10 smarts are key for these 3 injection services. When you’re coding in [...] - You Be the Coder:
Go Inside the Terms for Palsy Dx
Question: The provider performs a level-three established patient evaluation and management (E/M) service; the notes [...] - Reader Questions:
Hold the Line on Additional IV Infusion Time
Question: Notes indicate that my provider performed an intravenous (IV) infusion for therapy. The infusion lasted [...] - Reader Questions:
Track Telehealth Into 2021 for Coverage Updates
Question: Medicare implemented a lot of changes in coverage for telehealth in response to the public [...] - Reader Questions:
Get Hip to VEP Coding Exceptions
Question: Our provider performed a visual evoked potential (VEP) checkerboard test with interpretation and report. [...] - Reader Questions:
Use This ABN Form in 2021
Question: How do I know whether I’m using the correct advanced beneficiary notice (ABN) form [...]

