Urogynecology: Use Severity Modifiers With Physiotherapy Treatment to Complete Your Coding

Report the non-payable G codes to demonstrate the status of the treatment.
Therapy service G-codes require a severity modifier. Without the severity modifier, your claim will be denied. To avoid this frustration, review this case study and build up your physiotherapy coding knowledge.
Scenario: The urologist sees a female patient with stress urinary incontinence (625.6, Stress incontinence, female). The physician documents that the patient experiences leakage 80 percent of the time when she sneezes, laughs, or coughs. The goal of treatment is to decrease the patient’s leakage to less than 20 percent of the time.
Know When Each ‘G’ Code Applies
Reporting the functional limitation G codes became mandatory on July 1, 2013, says Michael A. Ferragamo, MD, FACS, clinical assistant professor of urology at the State University of New York at Stony Brook. “Claims submitted for outpatient physiotherapy services without a required functional G code/modifier will be returned to the provider unpaid,” he explains.
Specifically, the policy applies to physical therapy, occupational therapy, and speech-language pathology services furnished in hospitals, critical access hospitals, skilled nursing facilities, comprehensive outpatient rehabilitation facilities, rehabilitation agencies, home health agencies (when the beneficiary is not under a home health plan of care), and private offices of therapists, physicians, and non-physician practitioners. As in the above clinical scenario, for urology practices this most often applies to the physiotherapy treatment of urinary incontinence.
You will use three codes for urology:
Which ones you will report depend on which point in the treatment process you are reporting. You should include non-payable G-codes and modifiers on the submitted claims forms (a) at the first session; (b) at a minimum every 10th visit; and (c) at discharge.
“The guidelines state that you must report a G code for the first session and the last, and at least every tenth session, but you can report more often,” Ferragamo says. “Usually there are 4-8 sessions.”
Pick the Correct Modifier
These G-codes are “always therapy” codes which require a therapy modifier, Pamela R. West, DPT, MPH, of the CMS Center for Medicare Hospital and Ambulatory Payment Group, Division of Practitioner Services, said during a National Provider call.
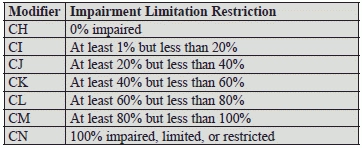
You’ll pick from the following ‘C’ modifiers:
“For the physiotherapy of urinary incontinence, most urologists will often use modifier CM, until the patient reaches their therapeutic goal, most often CI,” Ferragamo says.
The “C” severity modifiers reflect the score from a functional assessment tool or other performance measurement instrument, as appropriate. Use CMS’s guidance below.
Code the Case
Based on the above guidelines, for this case study, you would report the patient’s treatments as follows:
For the first treatment report the actual treatment using 97110 (Therapeutic procedure, 1 or more areas, each 15 minutes; therapeutic exercises to develop strength and endurance, range of motion and flexibility). Attach modifier GP (Services delivered under an outpatient physical therapy plan of care). Then, on the submitted claim, without charge, report G8990-CM-GP to indicate that the patient has just begun therapy and currently has symptoms 80 percent of the time. Next report G8991-CI-GP without charge for the final goal of therapy.
On re-evaluation if the patient has shown some improvement— for example, only having symptoms 50 percent of the time, halfway through treatment — again, report 97110-GP for the treatments. Then, add G8990-CK-GP. You will also document G8991-CI-GP as the expected final goal of your therapy.
Upon discharge, when the patient reaches the goal of less than 20 percent, report 97110-GP and G8992-CI-GP.