Medicare Compliance & Reimbursement
CMS Continues To Focus On Quality And Savings
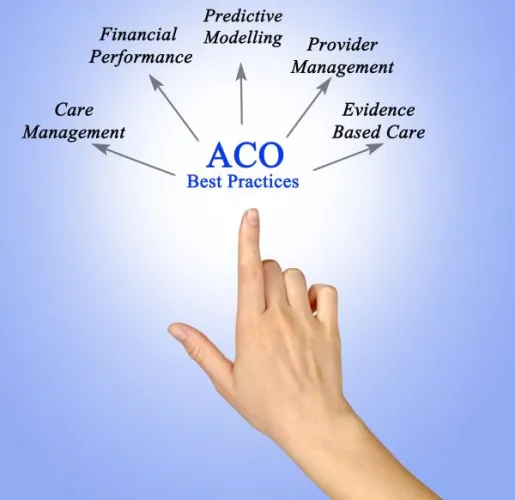
Recent payment models offer primary care, behavioral health expanded options. Not only did the pandemic shed light on the healthcare industry’s systemic issues with equity, but it also reminded many how critical a role primary care providers play and how important behavioral healthcare is for patients across all walks of life. Read on for a breakdown on three new payment models that aim to improve care and offer Medicare providers new opportunities. 1. Whole-person care is at the center of the IBH Model. In January, the Centers for Medicare & Medicaid Services (CMS) announced the Innovation in Behavioral Health (IBH) Model. The CMS Innovation Center will test the model, which will focus on gaps between physical and behavioral health and will be facilitated in the field via interprofessional care teams. “The systems of care to address physical and behavioral health conditions have historically been siloed, but there is a direct correlation between people with mental health conditions or substance use disorder and poor physical health,” asserts CMS Deputy Administrator and Innovation Center Director Liz Fowler in a release. “This model will bring historically siloed parts of the health system together to provide whole-person care – designed to keep people out of the emergency department, ensuring better care management and coordination, and improving their overall health.” Community-based providers and organizations — both public and private — will be the primary participants in the IBH Model. They will be incentivized “to work collaboratively to screen, assess, and coordinate between individuals’ physical and behavioral health needs,” CMS says. The agency will build on existing infrastructure, utilize health IT, and align the IBH Model with its “whole-person care” approach outlined in the CMS Behavioral Health Strategy. “While the IBH Model is limited to Medicaid and Medicare patients, it is likely that commercial payers may follow suit with similar programs, particularly if CMS shows successful outcomes,” predict attorneys Alexandra B. Maulden and Hannah E. Zaitlin with law firm Foley & Lardner LLP in online legal analysis. The IBH Model is slated for a fall 2024 start date and is scheduled to operate for up to eight years in at least eight states. 2. Competition and quality center around the new ACO PC Flex Model. Since the feds announced the HHS Initiative to Strengthen Primary Care, CMS has issued a plethora of policies and reforms. In March, CMS premiered the ACO Primary Care Flex Model (ACO PC Flex Model), which applies to primary care providers operating via Accountable Care Organizations and will be tested through the CMS Innovation Center within the Medicare Shared Savings Program (MSSP). A key component of the model will include a “a one-time advanced shared savings payment and monthly prospective primary care payments (PPCPs) to ACOs” to help with set up and ongoing resources, CMS says a fact sheet. “People whose primary care provider participates in the ACO PC Flex Model may get care in more convenient ways, like care based at home or through virtual means, extra help managing chronic diseases, and more preventive health services to keep them healthy,” said CMS Administrator Chiquita Brooks-LaSure in a release. “Not only will people with Medicare receive more coordinated, seamless care that addresses their unique needs, but CMS is supporting primary care clinicians and giving them more flexibility to provide person-centered care.” Smaller, low-revenues ACOs made up mostly of physicians will be the centerpiece of the new model, CMS indicates. The ACO PC Flex Model is voluntary and will run for five years, and CMS hopes to work with 130 ACOs via the program, which is scheduled to begin on Jan. 1, 2025. Applications for new and/or existing ACOs will be open from May 20, 2024 through June 17, 2024. 3. CMS proposes TEAM to bolster collaboration and equity. In its fiscal year (FY) 2025 Inpatient Prospective Payment System (IPPS) and Long-Term Care Hospital Prospective Payment System (LTCH PPS) proposed rule released in the Federal Register on April 10, CMS laid the groundwork for the possible mandatory payment model, Transforming Episode Accountability (TEAM) Model. TEAM “would incentivize coordination between care providers during a surgery, as well as the services provided during the 30 days that follow, and require referral to primary care services to support continuity of care and drive positive long-term health outcomes,” CMS says in a release. “This model would complement other CMS value-based care initiatives by promoting collaboration with accountable care organizations.” Environmental issues, including climate change, would also factor into TEAM outcomes and planning as CMS and HHS hope to garner data from participants to improve sustainability and collaboration while decreasing threats. “Before and after surgery, people on Medicare often experience fragmented care, especially following hospital discharge. This can lead to complications, prolonged recovery, unnecessary care, and even readmissions,” Fowler explains in a release. “By bundling all the costs of care for an episode, this proposed rule can incentivize care coordination, improve patient care transitions, and decrease the risk of an avoidable readmission.” CMS hopes to finalize TEAM in fall 2024. The mandatory payment model would run for five years, would include episode-based payment, and begin January 2026, agency guidance suggests.
Medicare Compliance & Reimbursement
- Payment Models:
CMS Continues To Focus On Quality And Savings
Recent payment models offer primary care, behavioral health expanded options. Not only did the pandemic [...] - MIPS Quiz:
Gauge Your Promoting Interoperability Savvy
Hint: Know the 4 PI objectives for PY 2024. If you think the Promoting Interoperability [...] - Part B Coding Coach:
+99459: 5 FAQs Clarify How to Use This Expense Only Code
Here’s what your physician’s documentation needs to include. Since January 1, you can use the [...] - Clip and Save:
Pocket This Primer On Informed Consent Forms
Pocket This Primer On Informed Consent Forms Critical: CMS revises interpretive guidance on informed consent. [...] - Reader Questions:
Understand The Rules On Reinstatement After Exclusion
Question: When an individual is excluded from participating in the Medicare program by the HHS Office [...] - Reader Questions:
Employ Protections for Patient Signatures
Question: In our recent risk evaluation, we discovered that the electronic signatures we and our patients [...] - Reader Questions:
Know When ‘Procedures’ Don’t Get Procedure Codes
Question: One of my providers recently removed an ear piercing, and he documented that “the post [...]

