What Would You Do?
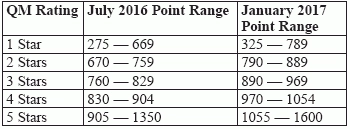
Question 1: Why do my correction/modifications get rejected? Answer 1: If the ASAP system rejects your correction or modification, this could be due to several different reasons. One reason is if the Assessment Submission and Processing (ASAP) system didn’t receive the original assessment, according to the Oklahoma State Department of Health (OSDH) Quality Improvement & Evaluation Service (QIES). Check to make sure ASAP received the original assessment, because you cannot modify an assessment if ASAP never received that assessment in the first place. The other possibility is that you might’ve internally changed coding items, dates, or personal identifiers for the resident, the OSDH QIES says. If this is the case, then ASAP won’t be able to locate that particular assessment. Question 2: How drastically have the Five Star Quality Rating scores changed since last year? Answer 2: The new Five Star Nursing Home Quality Rating cut-rate points have changes from July 2016 to the new ratings effective as of January 2017. According to the Five Star Technical User’s Guide (www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/nursinghomequalityinits/nhqiqualitymeasures.html), you can use the following table as a reference: Question 3: We’ve been noticing an increase in active urinary tract infections (UTIs) coded on MDS records. What should we do to figure out whether the coding is accurate and what’s going on? Answer 3: If you’re noticing an increase in active UTIs, you need to investigate this further and take a deep dive into the quality measure UTI triggers, advises Kris Mastrangelo, President and CEO of Harmony Healthcare International. First, you should ensure that the MDS coding of UTIs in item I2300 — Urinary Tract Infection (UTI) (Last 30 Days) meet all of the clinical criteria, Mastrangelo says. These criteria include: Second, double-check to ensure that only those infections that meet the above clinical criteria are coded on the MDS, Mastrangelo advises. Keep in mind that although clinicians may use the McGeer and Loeb criteria as the definitive authority on the presence of a UTI and whether to treat with antibiotics, this is a separate issue from whether you should code the UTI on the MDS. Nevertheless, if the infection did not meet the McGreers and Loeb criteria, the resident probably would not have been on medication and therefore would not be coded in item I2300, Mastrangelo notes. Finally, you should care plan for any condition that is a problem or concern, regardless of a diagnosis. Question 4: Should I code severe nosebleeds as internal bleeding for Problem Conditions in item J1550? Answer 4: You should check item J1550D — Internal bleeding if the resident has frank (such as bright-red blood) or occult (such as guaiac positive stools) internal bleeding during the seven-day look-back period. The RAI Manual includes in this item severe nosebleed (epistaxis) that requires packing. But you should not code easily controlled nosebleeds for item J1550D. Question 5: A resident fell and hit her head. She also lost consciousness and vomited. The emergency department visit indicated a discharge diagnosis of “minor head injury.” Should I code this as a fall with major injury or not? Answer 5: Since the resident lost consciousness, you should code it as a fall with major injury in J1900C, according to the Kansas Department for aging and Disability Services. Even though the diagnosis was “minor head injury,” you need to look to the coding instructions in the RAI Manual. The RAI Manual defines a major injury as including bone fractures, joint dislocations, closed head injuries with altered consciousness, and subdural hematoma.