What Do You Think?
Question 1: We admitted the resident to the nursing home on Jan. 17 and discharged to home on Jan. 21. Therapy staff evaluated the resident on Jan. 18 and treated him on Jan. 19 and Jan. 20, but staff did not provide any therapy on the day of discharge (Jan. 21). Does this qualify for a Short Stay since we provided no therapy on Jan. 21?
Answer 1: If you didn’t provide therapy because you discontinued all therapy services, then a Short Stay would not apply, according to the Kansas Department for Aging and Disability Services (KDADS).
Exception: “If the resident was still on therapy caseload and therapy expected treatment to continue but treatment was not given on the day of discharge for an unexpected reason, such as unexpected discharge, then a Short Stay is appropriate,” KDADS explained. In this case, you would “put dashes in the rehab end dates.”
Question 2: The resident was admitted with an unstageable pressure ulcer on his right hip. Three weeks later, staff debrided and reclassified it as a Stage 4 pressure ulcer. We listed the pressure ulcer as unstageable on the initial MDS assessment. On the current assessment, should we code the pressure ulcer as worsened?
Answer 2: No, you would not consider this pressure ulcer as new or worsened, according to a recent training presentation for Mountain-Pacific Quality Health by Jen Pettis, BS, RN, WCC with Abt Associates. You’ll code the pressure ulcer in item M0300D — Stage 4 Pressure Ulcers.
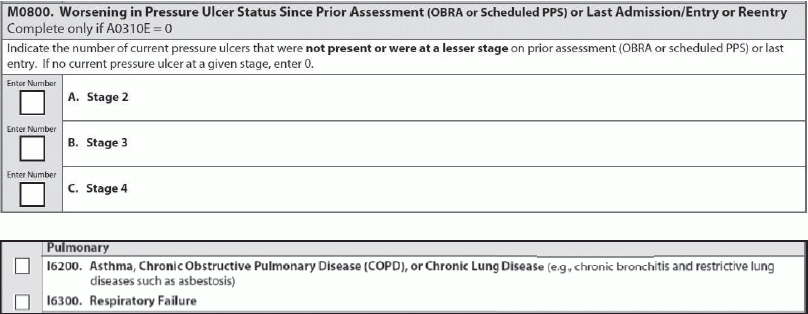
But you will not code this pressure ulcer in item M0800 — Worsening in Pressure Ulcer Status Since Prior Assessment (OBRA or Scheduled PPS) or Last Admission/Entry or Reentry.
Because this is the first time you’ve been able to stage the pressure ulcer, and the resident entered the facility with an unstageable existing pressure ulcer, the ulcer wouldn’t be considered new or worsening, Pettis explained. In other words, if a pressure ulcer is unstageable on admission and then becomes stageable, it’s not considered new or worsened unless it subsequently increases in stage.
Question 3: If a resident has a diagnosis of COPD but the physician says it’s stable (no meds or treatment given during the lookback period), would this be considered an active diagnosis?
Answer 3: To code a diagnosis as active in Section I — Active Diagnoses in the Last 7 Days, “you need that diagnosis from the physician in the last 60 days,” KDADS said. But in the seven-day lookback period, you also need “documented symptoms, abnormal lab or x-ray results, treatment or meds for the condition, or increased nursing monitoring.”
“If you don’t have some of these you cannot code it” for item I6200 — Asthma, Chronic Obstructive Pulmonary Disease (COPD), or Chronic Lung Disease, KDADS instructed. For more information, refer to the RAI Manual, pages I-7 and I-8.
Question 4: One of our residents was in the facility for only a short time. While with us, she required a variety of help for toileting: supervision twice, limited assistance twice, and extensive assistance twice. What should I code for self-performance for toilet use?
Answer 4: For Column 1 (Self-Performance) in item G0110I1 — Toilet use, you should code this situation as 2 — Limited assistance, according to Pettis. Here, you would apply the third part of the “Rule of 3,” because the resident didn’t have any particular level of assistance happen at least three times.
The third Rule of 3 states that if you have a combination of full staff performance, weight-bearing assistance and/or non-weight-bearing assistance, you should code limited assistance.
Tip: To reach this answer, you may want to use the ADL Self-Performance Algorithm on page G-8 of the RAI Manual for some help, Pettis suggested. When you have coding scenarios where the ADL happens three or more times, you probably don’t need much help if you’re following the Rule of 3. But the algorithm can help you figure out the correct coding for these types of less clear-cut coding scenarios.
Question 5: I’m a new MDS Coordinator at a nursing home, and I’ve noticed lots of different reports in CASPER. Which reports do I need to look at and which ones can I ignore, if any?
Answer 5: If you look under the Reports category in CASPER, you’ll see the subcategory “MDS 3.0 NH Provider,” which lists certain reports that you should periodically order and review, according to the Oklahoma State Department of Health (ODH) Quality Improvement & Evaluation Service. Reviewing the reports will help you to improve your accuracy for your quality measure (QM) reports.
These reports include: