MDS Alert
What Do You Think?
Question 1: Can I code barrier cream, A&D Ointment, and/or Eucerin cream or lotion in M1200H?
Answer 1: Yes, you can when you’re using these creams specifically to prevent or treat skin conditions, according to the Kansas Department for Aging and Disability Services (KDADS).
The RAI Manual (page M-40) instructions for coding Item M1200H — Applications of ointments/medications other than to feet state the following:
- Do not code application of ointments/medications (e.g., chemical or enzymatic debridement) for pressure ulcers here; instead, code these in M1200E — Pressure ulcer care.
- This category may include ointments or medications used to treat a skin condition (e.g., cortisone, antifungal preparations, chemotherapeutic agents).
- Ointments/medications may include topical creams, powders, and liquid sealants used to treat or prevent skin conditions.
- This category does not include ointments used to treat non-skin conditions (e.g., nitropaste for chest pain, testosterone cream).
Question 2: When is a default payment necessary?
Answer 2: Default payment is necessary only if the Assessment Reference Date (ARD) “is not set during the prescribed ARD window,” stated Carol Siem, MSN, RN, GNP-BC, RAC-CT, a Quality Improvement Program for Missouri’s Long-Term Care Facilities (QIPMO) clinical educator, in an instruction for the University of Missouri Health System’s Sinclair School of Nursing. “It has nothing to do with the completion or transmission of the MDS.”
Also, keep in mind that you must set the ARD for PPS assessments on the MDS form itself or in the facility software within the appropriate timeframe of the assessment type that you’re completing, Siem added.
Question 3: A resident was admitted to our facility for a respite stay under hospice (within a 30-day hospitalization), and the family wants her to receive skilled therapy for the admitting diagnosis of a s/p hip fracture under Medicare A. Can the resident receive skilled therapy services and be carried under hospice at the same time?’
Answer 3: Yes, says KDADS. According to the Medicare Benefit A Policy Manual (Chapter 9, Section 20.3), “a beneficiary could be in a SNF under the SNF benefit for a condition unrelated to the terminal condition and simultaneously be receiving hospice for a terminal condition.”
Important: Also be sure to include condition code 07 on the UB04 to reiterate that the hospice service is unrelated to the reason for the Medicare Part A stay, notes Marilyn Mines, RN, BC, RAC-CT, MDS Alert consulting editor and senior manager of clinical services for FROST Healthcare in Deerfield, Ill.
Question 4: I completed a 14-day MDS seven days prior to the change of therapy (COT) assessment. Can I use the 14-day interviews for Sections C and D? What is the rule for carrying over interviews for a COT?
Answer 4: When coding a COT, end of therapy (EOT), or start of therapy (SOT), you can code the interview items using the response that the resident provided on a previous assessment in a specific situation, according to KDADS. You can do so only if the date of the interview responses from the previous assessment were obtained no more than 14 days prior to the completion date for the interview items on the unscheduled assessment for which you will use those responses.
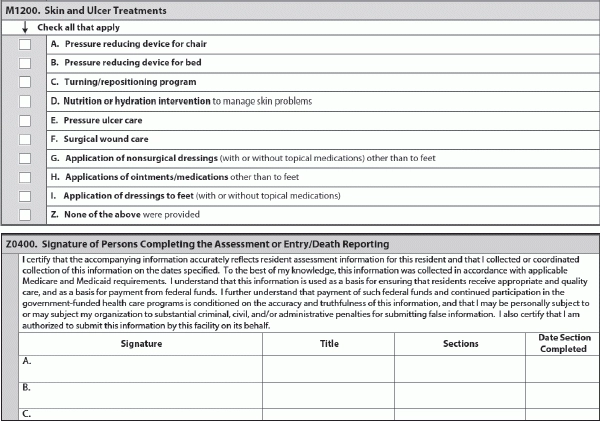
Find the completion date for the assessment in Item Z0400 — Signature of Persons Completing the Assessment or Entry/Death Reporting.
Question 5: The last day of the COT observation period was within the ARD window of a scheduled PPS assessment. When should I set the ARD?
Answer 5: “If Day 7 of the COT observation period falls within the ARD window of a scheduled PPS assessment, the SNF may choose to complete the PPS assessment alone by setting the ARD of the scheduled PPS assessment for an allowable day that is on or prior to Day 7 of the COT observation period,” Siem noted.
Also note: “The COT count starts on the day following the previous ARD in all cases, except in the case of the EOT-R,” KDADS said. “The EOT count starts the day of resumption.”
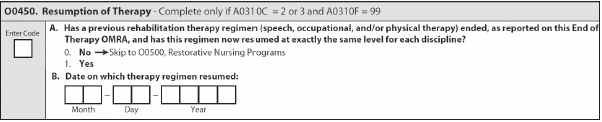
So if you’re resetting the seven-day rolling COT check on an EOT-R, Day 1 of the next COT check is the same day that therapy resumes. This is the date that you entered in O0450B — Date on which therapy regimen resumed.
MDS Alert
- Section H:
Don't Flush Away Your Urinary Incontinence Coding
Code this way even if the toileting trial doesn’t span entire look-back period. Both staff [...] - MDS 3.0:
Put Final Validation Reports To Work For You
Learn how to find missing validation reports, too. If you’re relying on your software to [...] - Tool:
Employ This Decision-Making Tool For Urinary Incontinence Solutions
You have more options than you think for assisting with dementia residents’ toileting. If your [...] - Section I:
Take 5 Steps To Smooth Your Transition To ICD-10
Check out newly revised ICD-10 educational materials. The looming implementation deadline for ICD-10 may seem [...] - Antipsychotics:
Heed Expert Tips For Proper Antipsychotic Medication Coding
Make sure you’re coding medications received, even outside your facility. With all the scrutiny that [...] - What Do You Think?
Question 1: Can I code barrier cream, A&D Ointment, and/or Eucerin cream or lotion in [...] - Industry News to Use:
Get Ready For Sweeping Changes To LTC Regulations
Plus: NPUAP criticizes ‘hand check method’ for bottoming out. You could soon be faced with [...]

