MDS Alert
Use These Decision Points To Complete J0200
Don’t discount all residents with cognitive impairment.
Gathering resident information on pain from staff observations isn’t as accurate as getting it from the resident herself. And if you’re skipping the Pain Assessment Interview and going straight to the Staff Assessment for Pain in Section J, you’d better have a very good reason.
According to the Centers for Medicare & Medicaid Services (CMS), you should use staff observations for pain behavior only if a resident cannot communicate in one of these ways:
· Verbally;
· With gestures; or
· In writing.
Check B0100 Comatose on the resident’s MDS — if it’s coded 1 Yes, you have a valid reason to skip the interview and go on to the Staff Assessment for Pain section, CMS notes. And check A1100 Language to determine whether the resident wants or needs an interpreter, and then provide one for the interview.
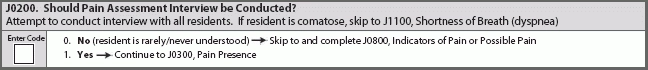
In J0200 (Should Pain Assessment Interview be Conducted?), check 0 No if the resident is rarely or never understood, or if the resident requires an interpreter but one is not available. Check 1 Yes if the resident is at least sometimes understood and an interpreter is present or not required.
“I would strongly encourage you to really look at this, though,” said Ann Spenard, MSN, RN, C, vice president for operations at Qualidigm, based in Rocky Hill, CT, in a CMS instructional session. You shouldn’t simply rely on Section B to tell you definitively whether the resident could complete the Pain Assessment Interview. If you weren’t the staff member who completed Section B for that resident, go talk it over with the person who did.
Bottom line: “If there’s any level of the person being understood, we want you to try to do the pain interview,” Spenard stressed.
MDS Alert
- Section I:
Active Diagnoses: How To Juggle 2 Look-Back Periods
Is it really an active or an inactive diagnosis? MDS 3.0 coding is frustrating enough [...] - Nutrition:
4 Ways You Might Be Wrecking Your K0510 Coding
Hint: Your biggest battle may lie with K0510D Therapeutic diet. The K0510 Nutritional Approaches section [...] - Meet All Conditions To Code I2300
Beware of UTI look-back exception for active diagnoses. As if the double look-back periods for [...] - Pain Assessment:
Follow 7 Tips To Ensure Pain Assessment Interview Flows Smoothly
Make sure you’re coding J0850 this way. You can make a lot of minor — [...] - Use These Decision Points To Complete J0200
Don’t discount all residents with cognitive impairment. Gathering resident information on pain from staff observations [...] - M0300:
How To Report The 'Unstageable' Pressure Ulcer
Check out these 4 scenarios to code tricky situations. You may not be able to [...] - Section L:
Quick Tips: Don't Let Oral Health Assessments Discourage You
How to make uncooperative residents relaxed and compliant. Performing oral health assessments can seem daunting, [...] - What Do You Think?
Question 1: I live in the Midwest and my facility needed to be evacuated secondary [...] - Industry News to Use:
You No Longer Need An Inactivation Request For Certain MDS Errors
Plus: Get ready for SNF pay increase? The Centers for Medicare & Medicaid Services (CMS) [...]

