Evaluate Bed Rail Usage, Stat
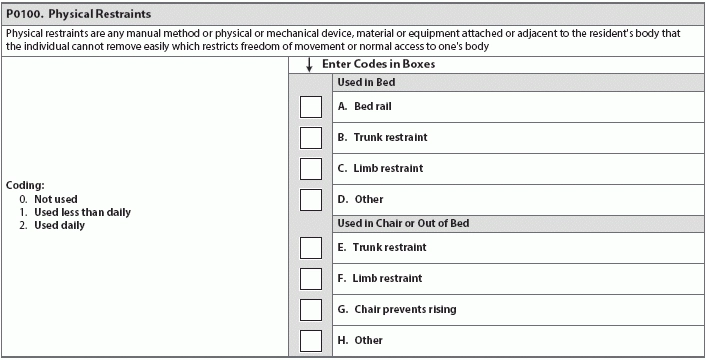
Surveyors now have bed rail-specific FTags. Bed rails and the risk for entrapment have been on the radar for skilled nursing facilities, resident advocates, and healthcare personnel for over a decade now, but now's a great time to take another look at how you're evaluating bed safety. With Section P (Restraints and Alarms) now focusing on further reducing restraint and alarm use, bed entrapment is receiving new attention from facility staff and surveyors alike. First of all, if bed rail usage is currently in use or being considered for an individual resident, the interdisciplinary team should work together to decide whether a particular resident truly needs bed rails. Neither the Food and Drug Administration (FDA) nor the Centers for Medicare and Medicaid Services (CMS) ban bed rails, but CMS considers bed rails a physical restraint in certain situations, depending on an individual resident's cognitive and physical realities. For example, some residents may increase their independence and mobility from the use of a bed rail, and others may be endangered by its presence. The RAI Manual defines bed rails as "any combination of partial or full rails (e.g., one-side half-rail, one-side full rail, two-sided half-rails or quarter-rails, rails along the side of the bed that block three-quarters to the whole length of the mattress from top to bottom, etc.)." The most recent data available through the FDA's Consumer Product safety Commission (CPSC) suggests that 25 people were injured or died from bed rail entrapment in nursing homes and 15 in assisted-living facilities from January 2003 through September 2012. CMS notes the danger and instructs surveyors to be on the lookout for unnecessary or inappropriate bed rail usage. Beware: Surveyors can levy several FTags with language specific to bed rail use they consider inappropriate or unnecessary. Not all bed rails fit all frames. Using bed rails improperly, including mismatching rails to a frame or using with other devices that remain in place when the rail is removed, can further exacerbate the potential risks, according to CMS's State Operations Manual Appendix PP. Appendix PP warns against the very real dangers of using bed rails: "In many cases, the risk of using the bed rails may be greater than the risk of not using them as the risk of restraint-related injury and death is significant. For example, a resident who has no voluntary movement may still exhibit involuntary movements. Involuntary movements, resident weight, and gravity's effects may lead to the resident's body shifting toward the edge of the bed, increasing the risk for entrapment, when bed rails are used." The interdisciplinary team, including nursing, maintenance, and therapies should conduct an initial bed assessment, along with annual bed inspections of all bed rail usage, bed frames, and bed accessories to detect risk of entrapment, says Kris Mastrangelo, president and CEO of Harmony Healthcare international in Topsfield, Massachusetts. For many residents, the risks of bed rails often outweigh the benefits. Bed rails can cause suffocation, strangling, death, falls, skin injuries, agitated behavior, feelings of isolation, and restriction of movement, Mastrangelo says. Some residents may be able to use a bed rail for assistance when transferring in and out of bed, or feel more secured by its presence, which are both benefits, she notes. Plus, bed rails can also prevent falls when residents are transported via bed. Surveyors will be looking to make sure that if they see bed rails, the facility has gone through all of the proper measures before implementing their use. These measures include investigating "appropriate alternatives" and, if using bed rails, making sure that staff evaluates the resident in question for entrapment. Surveyors will be checking to see that the bed rails are medically necessary (with supporting clinical documentation), as well as evaluating the bed rails to see whether they are correctly installed, used, and maintained. If a resident is deemed to need bed rails for medical reasons, make sure that staff monitors that resident closely. Note: The new Long Term Care Survey Process calls for surveyors to be especially comprehensive in their observations and evaluations, even checking to see how a resident using bed rails contacts staff for assistance and to have staff ask the resident to demonstrate releasing the bed rails. Some residents may be able to use bed rails to aid in their mobility, such as repositioning their bodies while in bed or as a handhold for getting into or out of bed. If a resident has a bed rail for mobility purposes, and the bed rail meets the definition of a restraint, the RAI Manual still requires coding the device as a restraint in P0100A (Physical Restraints, Bed rail). See Chapter 3 P-5 in the RAI Manual for more information. Include the implementation of a bed assessment for all new admissions, Mastrangelo advises. Remember: Surveyors may levy citations that include bed alarms, which are now considered restraints, she adds. Resource: You can find Harmony Healthcare International's exclusive 13-page comprehensive bed assessment form at http://www.harmony-healthcare.com/blog/bed-inspections-risk-for-entrapment.