Don't Sink Your Quality Scores -- Tread Carefully When Coding M0800
How to handle unstageable pressure ulcers in Item M0800.
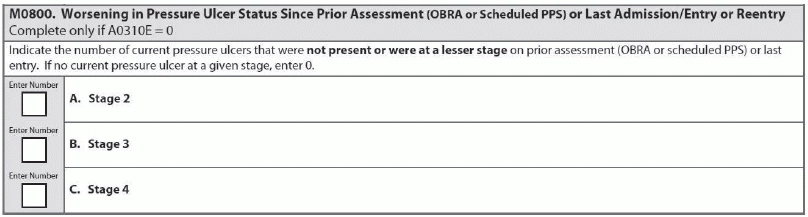
Item M0800 — Worsening in Pressure Ulcer Status Since Prior Assessment (OBRA or Scheduled PPS) or Last Admission/Entry or Reentry is one of those MDS 3.0 items that can put a dent in your facility’s Quality Measure scores. So all the more reason to make sure your coding is accurate and that you aren’t coding pressure ulcers that haven’t actually “worsened.”
Here are four expert tips to help you understand how to correctly code M0800:
Tip #1: Why Merged Pressure Ulcers Don’t Belong in M0800
Example: Two pressure ulcers at different stages (Stage 2 and Stage 3) have merged. Do you code this as “worsening” in M0800?
Answer: You should not consider a merged pressure ulcer “worsened” only because its area is now larger, according to the Pennsylvania Department of Health’s (PADH) RAI Spotlight.
“If a Stage 2 and a Stage 3 ulcer merged, the classification of this united ulcer would be based on the depth of the Stage 3 portion of the wound,” the PADH said. You must stage a pressure ulcer by determining its deepest anatomical stage. “Worsening” means that a pressure ulcer has progressed to a deeper level of tissue damage, therefore you would stage it at a higher number using the numerical scale of one to four.
In this scenario, both ulcers were present previously, meaning they are not new in this observation period. Also, the overall highest numerical stage has not increased. “In this unusual situation, the merged ulcer should not be considered as ‘worsened’ at M0800,” PADH instructed.
Tip #2: When Debrided Ulcers Could ‘Worsen’
Example: A resident’s Stage 3 pressure ulcer is debrided and now classifies as a Stage 4. Should you consider this ulcer “worsened” at M0800?
Solution: If you previously numerically staged the pressure ulcer and the debridement identified a deeper-stage wound, you would consider it as worsened, PADH noted. This is simply because the pressure ulcer has increased in numerical stage.
Tip #3: Avoid Blame When Worsening Occurs Outside Facility
Example: A resident discharges from your facility for a hospital stay. During the hospital stay, the resident’s pressure ulcer worsens to a more severe stage, which you notice upon the resident’s return to your facility.
Answer: If a pressure ulcer worsens to a more severe stage during a hospital admission, you should code it as “present on admission,” according to the University of Missouri-Columbia’s Sinclair School of Nursing. Do not include the pressure ulcer in your counts of worsening pressure ulcers.
The coding for M0800 and M0300 — Current Number of Unhealed Pressure Ulcers at Each Stage truly goes hand-in-hand, according to a blog posting by Topsfield, Mass.-based Harmony Healthcare International. So you must ensure that the resident’s complete admission skin assessment is well-documented, including the accurate staging of any pressure ulcers. You would consider a pressure ulcer as not present on admission (i.e., in-house acquired) if it is new or worsens in your facility.
“Although documenting whether a pressure ulcer is present on admission (in M0300) does not impact the Quality Measures, the Stage 2 through 4 pressure ulcers documented in M0300 do, as does coding indicating a pressure ulcer is new or worsening in M0800.”
Tip #4: Handle M0800 Coding for Unstageable Ulcers This Way
Example: The resident is admitted to your facility with an unstageable pressure ulcer. After debridement, the pressure ulcer classifies as a Stage 4.
Answer: If you listed the pressure ulcer as unstageable on the initial MDS assessment, you would not code it as worsening on the subsequent assessment, according to the RAI Manual. This is the first numerical staging since the debridement.
Or, say a resident develops a Stage 3 pressure ulcer while in your facility. The wound bed then covers with slough, so you code it on the next assessment as unstageable due to slough. After debridement, you reassess the pressure ulcer and determine that it is yet again a Stage 3.
In this case, you would still not code the pressure ulcer as worsened (M0800B = 0) because the pressure ulcer’s numerical stage is the same as it was prior to the period when it became unstageable, the RAI Manual explains.
Remember: The suggestions in F314 indicate that a “significant number of pressure ulcers develop within the first four weeks after admission to a long-term care facility. Therefore, clinicians recommend using a standardized pressure ulcer risk assessment tool to assess a resident’s pressure ulcer risks upon admission, weekly for the first four weeks after admission for each resident at risk, then quarterly, or whenever there is a change in cognition or functional ability.”
“This practice is often ‘expected’ by surveyors when determining whether the development of the pressure ulcer was avoidable or not,” stresses Marilyn Mines, RN, BC, RAC-CT, MDS Alert consulting editor and senior manager of clinical services for FR&R Healthcare Consulting Inc. in Deerfield, IL.