Confusing a scab as eschar could land you with an underserved Stage 4.
Now is the time to brush up on your pressure ulcer coding, because surveyors are placing a renewed focus on this section of the MDS, thanks to the latest tallied results from the MDS Focused Surveys. And experts believe that you need to study up on some pressure ulcer fundamentals.
The Centers for Medicare & Medicaid Services (CMS) recently released a memo detailing the results of the Fiscal Year (FY) 2015 MDS Focused Surveys (see “MDS Focused Surveys: Your Coding Accuracy Is Coming Under Fire,” MDS Alert, Vol. 14, No. 11, page 131). In the MDS Focused Surveys, CMS discovered that surveyors frequently cited F-278 — MDS Accuracy as well as F-314 — Treatment/Services to Prevent Pressure Ulcers.
Beware: The F-278 deficiencies that surveyors cited for MDS accuracy most commonly linked to coding errors in specific areas, and pressure ulcer coding ranked among the top seven areas.
According to CMS, surveyors found in these cases that facilities’ coding was inconsistent for residents both with and without pressure ulcers, and that pressure ulcers weren’t coded at the correct stages. Also, surveyors found that facilities coded the incorrect number of pressure ulcers and coded ulcers as healed when they were not healed.
What Really is a Pressure Ulcer?
Clinicians tend to have certain fundamental questions and misunderstandings when it comes to identifying and coding pressure ulcers in Section M — Skin Conditions. One key question is whether a wound is in fact a pressure ulcer when it arises due to a combination of factors, noted elizabeth ayello, PhD, Rn, aCns-BC, CWon, etn, MaPWCa, Faan, in a CMS educational session.
To answer this question, you need only to look to the RAI Manual, which is very clear. The Manual states that if an ulcer arises from a combination of factors which are primarily caused by pressure, then you should code the ulcer in Section M as a pressure ulcer.
Another often miscoded situation is when a resident has a pressure ulcer on his lip or mucosa. You should not code this in Section M, because the mucosa is not skin — instead, you would code this in item L0200C — Abnormal mouth tissue.
Why? “Mucosa is different from skin; mucosa does not keratinize,” Ayello explained. “So you cannot compare what’s going on with the mucosa to the skin because, remember, staging is based on anatomical types of tissue. You don’t have the same layers in mucosa that you have in skin.”
Also, pressure ulcers that are closed by a flap or a graft tend to trip coders up. If a pressure ulcer is surgically closed with a flap or graft, you should code it as a surgical wound in M1040E — Surgical wound(s) and not as a pressure ulcer. Even if the flap or graft fails, you would still continue to code it as a surgical wound until it’s healed.
“The concept that I try to teach people is a wound could start out as one etiology on the wound bed preparation model, and then it could become another etiology,” Ayello noted. “Because of what’s going on either with the resident, condition, or because of the treatment.” And the flap or graft scenario is an example of where the wound etiology changed due to the treatment.
Follow the Keys to Staging
A fundamental convention in the pressure ulcer items in Section M is the “deepest anatomical stage.” For pressure ulcer staging, you want to know what type of tissue, because staging is based on the deepest anatomical type of soft tissue damage, Ayello said. The deepest anatomical stage or “anatomical depth” is based on the type of tissue, not on a measurement in centimeters.
Crucial: Another issue is the fact that the definitions of the different pressure ulcer stages in the RAI Manual are adapted, not adopted, from the National Pressure Ulcer Advisory Panel (NPUAP), Ayello stressed. Of course, the RAI Manual and the NPUAP staging descriptors are the same for the most part, but there are differences that could impact your coding.
And your team can always use the NPUAP definitions in their clinical documentation, but you must use the CMS RAI Manual definitions for coding purposes on the MDS 3.0.
What’s the biggest difference between the NPUAP definitions and those in Section M? Actually, the only difference is on how to code blister pressure ulcers on the MDS versus the NPUAP definitions, Ayello said. (For more on coding blister pressure ulcers, see “Overcome 3 Pressure-Ulcer Staging Stumbling Blocks” on cover page.)
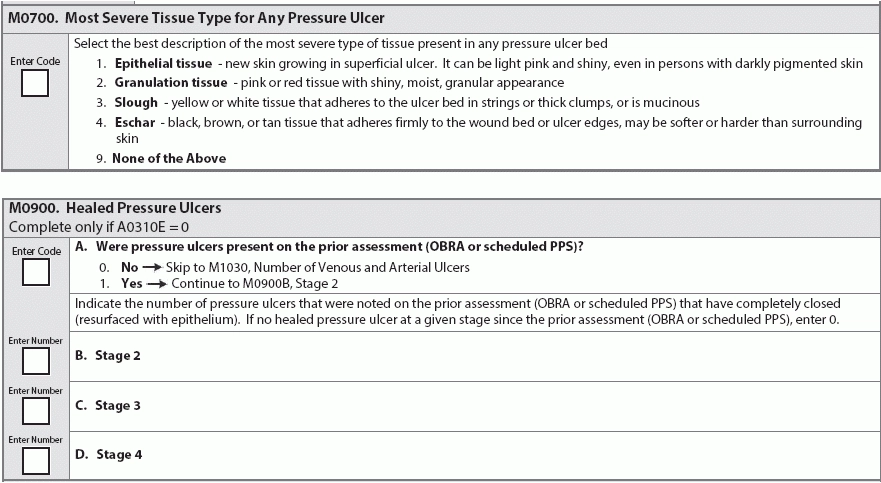
Another problem: Don’t confuse scabs with eschar, because this could cause you to incorrectly code a healing wound with a Stage 4 pressure ulcer and a high code in item M0700 — Most Severe Tissue Type for Any Pressure Ulcer.
Scabs are made up of dried blood cells and serum, sitting on top of the skin and forming over exposed wounds, Ayello said. Scabs are evidence of wound healing, while eschar is a collection of dead tissue within the wound that is flush with the wound’s surface. If a Stage 2 pressure ulcer has a scab (not eschar), this means it’s a healing Stage 2 ulcer and therefore your staging should not change.
Decode the ‘No Back-Staging’ Rule
You can’t back- or reverse-stage pressure ulcers, meaning that once you code a pressure ulcer as a Stage 4, for instance, you cannot then reclassify it as a Stage 3, Stage 2 and so on as it heals. Simply put, once a pressure ulcer is a Stage 4, it’s always going to be a Stage 4.
The wound “will always be considered a healing Stage 4 as it is counted on the MDS,” Ayello instructed. And once the pressure ulcer is completely healed, you can then code it in M0900D — Healed Pressure Ulcers, Stage 4.
An additional tricky coding situation is when a pressure ulcer reopens. If a pressure ulcer that you coded on the previous MDS heals and then reopens at the same stage by the next MDS, you may wonder what you should code as the date of origin — the original date or the date the wound reopened.
In this case, you would use the original date, because this pressure ulcer isn’t considered to have been healed, according to a recent american association of nurse Assessment Coordination (AANAC) Q&A with MDSexpert Rena shephard, MHa, Rn, RaC-Mt, Dns-Mt.
The RAI Manual states: “If the prior assessment documents that a pressure ulcer healed between MDS assessments, but another pressure ulcer occurred at the same anatomical location, do not consider this pressure ulcer as healed. The reopened pressure ulcer should be staged at its highest numerical stage until fully healed.”
Gauge Pressure Ulcer Risk
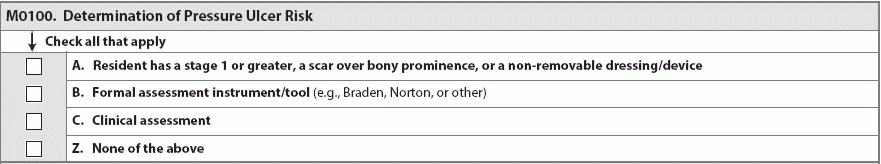
Yet another important element in your Section M coding is determining whether a resident is at risk for developing pressure ulcers, which you must code in item M0100 — Determination of Pressure Ulcer Risk. For this item, you shouldn’t consider just one factor, but instead you should take a holistic, “multifactor” approach, Ayello stressed.
“There’s not one thing that puts a resident at risk for developing a pressure ulcer,” Ayello stated. Your multifactorial process should involve:
Essential: You must perform a head-to-toe skin assessment, Ayello urged. Make sure you have adequate lighting for your visual assessment and actually palpate the resident’s skin. Pay special attention to bony prominences and pressure-bearing areas like the sacrum, heels, ankles, and skin beneath medical devices.
Factors for pressure ulcer risk include cognitive impairment, urinary and/or fecal impairment, as well as under-nutrition, malnutrition and hydration deficits. Medications, immobility, comorbidities, Braden scores, current health acuity, and use of medical devices can all also contribute to a resident’s risk for developing pressure ulcers.
The presence of healed pressure ulcers (especially Stage 3 or 4 ulcers) is a big risk factor, due to the greater chances of those ulcers reopening. The tensile strength of a healed pressure ulcer is only 80 percent of normal skin tensile strength, Ayello pointed out.
Resource: To access a recording of the CMS educational session on Section M, visit http://surveyortraining.cms.hhs.gov/Courses/126/SectionMVideo/SectionMVideo.html.