MDS Alert
Take The 'Ouch' Out Of Your Resident Pain Assessments
Find out the best way to deal with pain-related QM triggers.
If yours is like most nursing facilities, you and your staff likely spend a lot of time managing residents’ pain. But if you’re not assessing a resident’s pain frequently enough, you could be missing out on key feedback for treatment and well-being.
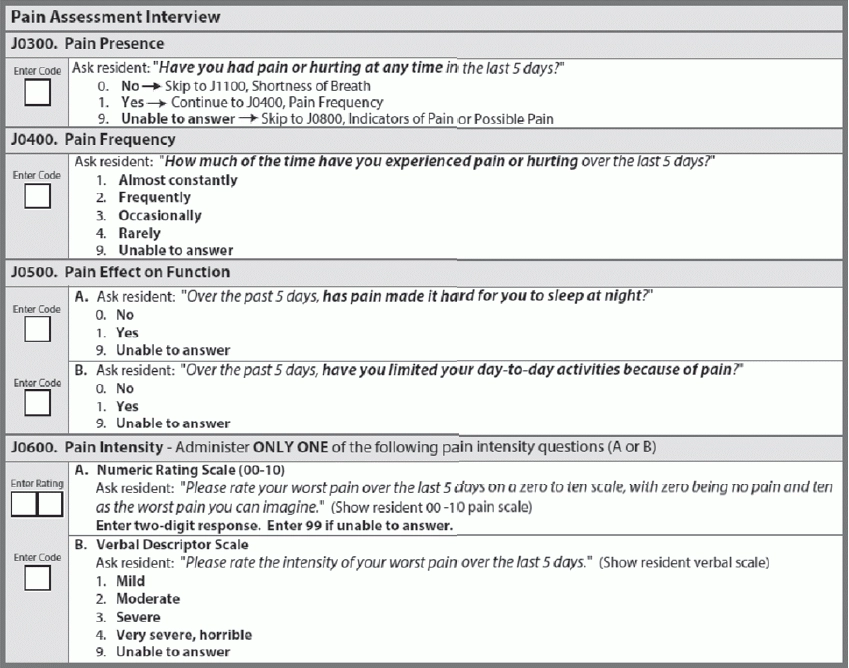
When coding the pain items in Section J — Health Conditions, you should use the resident pain-assessment interview instead of the staff assessment if at all possible. Resident self-reporting is the most reliable means for assessing pain, according to a recent training by Becky LaBarge, RN, RAC-MT for Leading Age Kansas.
Best: Assess for Pain More Frequently
You have to interview residents regarding pain upon admission, quarterly, and with significant changes, says Melody Schrock, BSN, RN, Clinical Educator with the Quality Improvement Program for Missouri’s Long-Term Care Facilities (QIPMO). “But what happens between these assessments?
You should encourage and complete more frequent assessments, ideally at least monthly with long-stay (more than 100 days) residents and weekly for short-stay (less than or equal to 100 days) residents, Schrock recommends. “This develops a relationship and lets the resident know you are sincere and empathetic to [her] pain management.”
How? You can increase the frequency of pain assessments in your facility by including them with medication passes, Schrock suggests. “Include team members from all departments when completing staff assessments of pain; our elders don’t just talk to nursing department staff.”
Remember: For your regular assessments, however, conduct the pain interview close to the end of the five-day look-back period, preferably on the day before or the day of the Assessment Reference Date (ARD), LaBarge advised.
Beware of QM Triggers
There are both short-stay and long-stay quality measures (QMs) for pain (Percent of Residents Who Self-Report Moderate to Severe Pain).
According to Schrock, coding Item J0400 — Pain Frequency as either 1 — Almost constantly or 2 — Frequently will trigger the pain QM, as well coding Item J0600 — Pain Intensity as 05 through 10 (on J0600A — Numeric Rating Scale) or as 2 — Moderate, 3 — Severe, or 4 — Very severe, horrible (on J0600B — Verbal Descriptor Scale).
Mistake: But don’t shy away from reporting higher levels of pain when the resident identifies them. You must document what the resident reports.
Even though this will trigger on the QM, you can ensure that justification is present during surveyor reviews by following up the pain scoring “with an in-depth note describing what actions have been taken to address pain, non-medicinal means as well as medication regimen reviews, changes, and pain relief interventions,” Schrock advises.
Also, stay alert to the relationships among QMs, such as how pain could impact depression, LaBarge added. “The effects of unrelieved pain impact the individual in terms of functional decline, complications of immobility, skin breakdown, and infections.”
Bottom line: “Pain, contrary to common myth, is not a natural part of aging,” Schrock reminds. “While it does follow a number of diagnoses, we must proactively seek out the pain residents in our homes experience. We must find its source, the kind of pain and its intensity, and ultimately, the elder’s perception of that pain.”
Resource: Schrock points to the Advancing Excellence toolkit found at www.nhqualitycampaign.org/goalDetail.aspx?g=pain#tab3 as a good resource to “explore goals, identify base line, examine process, create improvement, engage, monitor and sustain, and ultimately, celebrate your success.”
MDS Alert
- Assessments:
How To Avoid These 6 Most-Common SCSA Mistakes
Don’t get tunnel vision — look for improvements, not just declines. The right situation in [...] - Surveys:
Heed Expert Tips For Annual Survey Prep & Conducting Mock Surveys
Why the QIS tools should be your basis for a mock survey. Managers are on [...] - Look For These SCSA-Triggering Scenarios
Overall deterioration may include a pattern of changes. When deciding whether to initiate a Significant [...] - Tool:
Use This Checklist To Get Prepared For Your Annual Survey
Make sure you have these crucial documents on-hand for surveyors. If you’re wondering which key [...] - MDS 3.0:
Prepare Early For October 2016 MDS 3.0 Changes
You won’t find these Section C items in the updated RAI Manual. Despite promising substantial [...] - Quality:
Your PEPPER & Five-Star Preview Report Are Now Available
Get ready for new quality measures to make a big splash in July. You can [...] - Section J:
Take The 'Ouch' Out Of Your Resident Pain Assessments
Find out the best way to deal with pain-related QM triggers. If yours is like [...] - What Do You Think?
Question 1: What happens if a staff member documents in her ADL charting that a [...]

