Long-Stay QM: How J0300-J0600 Coding Impacts Your Quality Scores
Find out why you should use the Numeric Rating Scale whenever possible.
When it comes to residents’ reports of pain, the way you code the MDS could make your quality measure (QM) scores take a nosedive. But with a few MDS coding strategies and a solid understanding of how to calculate this QM, you can ensure that your quality scores travel in the right direction.
Key: A resident’s self-reporting is the most reliable means for assessing pain, according to a recent presentation for the Pennsylvania Department of Health by Catharine Petko, RN, BSN, Senior Nurse Consultant with Myers and Stauffer LC. That’s why the Centers for Medicare & Medicaid Services (CMS) includes this data point among the QMs that affect your Nursing Home Compare and Five-Star Quality Rating scores.
There is both a short-stay and a long-stay QM for residents who self-report moderate to severe pain. For the long-stay QM, the measure aims to capture the percent of long-stay residents who report either:
1. Almost constant or frequent moderate to severe pain in the last five days; or
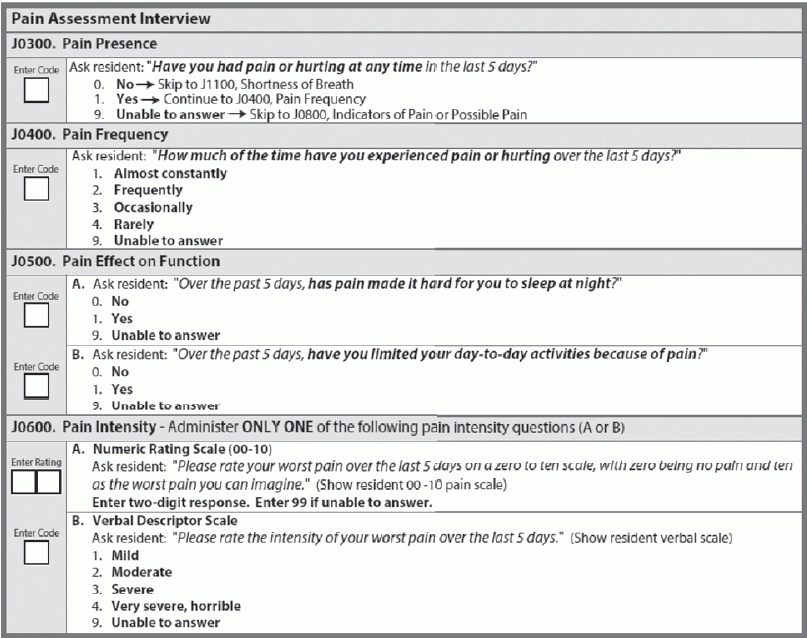
What MDS Data the QM Involves
To calculate the QM, CMS specifies certain criteria for the resident populations included in the numerator and in the denominator. First, the numerator includes long-stay residents with a selected target assessment meeting either or both of the following two conditions:
1. Resident reports almost constant or frequent moderate to severe pain in the last five days with both:
a. J0400 — Pain Frequency coded as 1 — Almost constantly or 2 — Frequently; AND
2. Resident reports very severe/horrible pain of any frequency with J0600A coded as 10 on the pain scale, or J0600B coded as 4 — Very severe, horrible.
The denominator includes all long-stay residents with a selected target assessment, except for those with the following exclusions:
o J0200 — Should Pain Assessment Interview be Conducted? isn’t completed (0, -, ^).
o For residents coded in J0300 as 1, ANY of the following are true:
§ J0400 isn’t completed (9, -, ^).
Perfect Your Pain Assessment Coding
Important: The lookback period for the pain assessment is five days, but ideally the Assessment Reference Date (ARD) plus four days, Petko noted. You should conduct the pain interview as close to the end of the general observation period as possible, preferably the day before or the day of the ARD.
“The pain interview has to be done on time and no later than the ARD,” agrees David Johnson, NHA, RAC-CT, Senior Quality Improvement Specialist with IPRO. “The easiest way to illustrate this is that if you have a receipt for a tax-deductible item dated this year, you can’t apply it to last year’s tax return. The ARD on the MDS is the end date for that MDS.”
Also, you must ask the resident each item (J0300 through J0600) directly and in the order the items appear on the MDS, Petko advised. And use the resident’s terminology for pain, such as “hurting,” “aching,” or “burning.”
Pitfall: When you’re coding frequency in J0400, beware that there are no definitions available for the choices, “so the definition is whatever the resident reports,” Johnson states. And remember that the first two choices will make the resident eligible for a possible trigger to the QM.
And when you’re coding J0300, you should code for the presence or absence of pain regardless of any pain management efforts, Petko said. So if the resident tells you that he has had no pain, you should code J0300 as 0 — No, even if the reason he had no pain was because he received pain management interventions like pain meds.
Choose Your Pain Scale Carefully
For pain intensity (J0600), you have a choice of which scale you want to use, the numeric scale or the verbal descriptor scale, Johnson says. You must use one of these scales, not both, and try to use the same scale from one MDS record to the next with each resident.
Interestingly, the numeric scale could cause a possible trigger only if the resident reports a level of “05” or greater, but the verbal descriptor scale could cause a trigger for any code greater than 1 — Mild, Johnson points out.
Best bet: “My suggestion is that you use the numeric scale,” Johnson advises. “It is the first choice offered on the MDS with a little more opportunity for clarification. On the descriptor scale, there are no offers of definition, so the descriptor scale is whatever is reported by the resident.”
Scenario: If you use a pain scale illustrating levels of pain numbered 0 through 10, you should illustrate “moderate” pain in the middle as 5, because this point on the numeric scale triggers the QM. So “0” on the scale would be “no pain” and “10” would be the “worst possible pain.”
Moderate pain (indicated by 5 on the numeric scale) identifies as a key area in your pain management program, Johnson notes. This is because the RAI Manual states that most residents with moderate to severe pain will require regularly dosed pain medication, with some requiring additional PRN pain medications for breakthrough pain — but some residents with intermittent or mild pain may have orders for PRN dosing only.
This is important because “if you review your data and find that residents triggering for a minimum of 5 are on only a PRN pain medication, that is an area for possible focus,” Johnson says. “They should be considered for a regularly dosed pain medication because at a moderate level of pain, you are not managing their pain with a PRN med — they are managing their pain because you are waiting for their ‘report’ of that pain.”
2. Any very severe/horrible pain in the last five days.
b. J0600A — Pain Intensity, Numeric Rating Scale coded as 05, 06, 07, 08 or 09 on the pain scale, OR J0600B — Pain Intensity, Verbal Descriptor Scale coded as 2 — Moderate or 3 — Severe.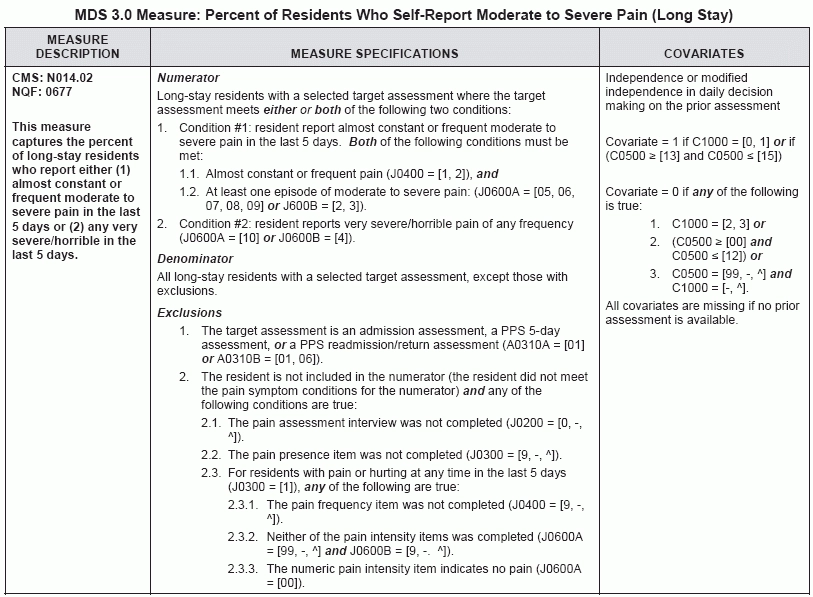
o J0300 — Pain Presence isn’t completed (9, -, ^).
§ J0600A isn’t completed (99, -, ^) AND J0600B isn’t completed (9, -, ^).
§ J0600A is 00 on the numeric rating scale.