Prioritize Language as Key to PDPM Accuracy
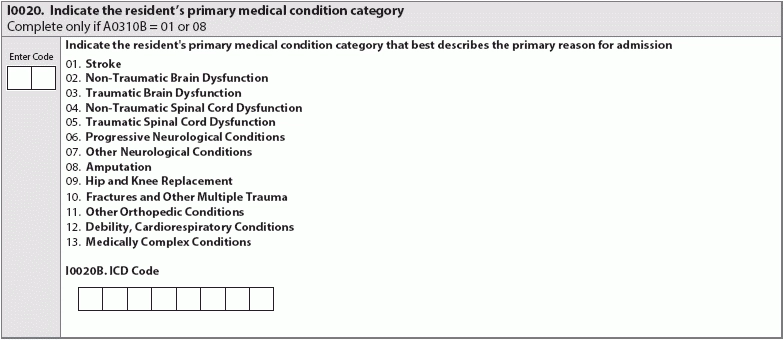
Know which diagnoses CMS believes appropriate for a nursing facility stay. The fact that many nursing facility residents will have multiple health conditions or comorbidities is simply a reality. A resident may have multiple conditions that require more intensive nursing or special attention while the resident is living in your nursing facility. So figuring out the correct way to code MDS item I0020 (Indicate the resident’s primary medical condition category) may involve sifting through multiple diagnoses. Prioritize documenting the reason, via ICD-10 code, that the resident ended up in the facility. Separate Active Diagnoses The Centers for Medicare & Medicaid Services (CMS) intends the MDS to reflect an accurate picture of a resident’s overall health. Section I, which focuses on active diagnoses, is supposed to show how the resident’s various ailments present a need for care. The items vary from the reason for admission to other active diagnoses in the prior seven days. “The items in this section are intended to code diseases that have a direct relationship to the resident’s current functional status, cognitive status, mood or behavior status, medical treatments, nursing monitoring, or risk of death,” the Resident Assessment Instrument (RAI) Manual says, on page I-5. However, with the new requirements for Medicare Part A residents under the Patient-Driven Payment Model (PDPM), some nurse assessment coordinators may be confused about how to figure out the primary diagnosis when a resident presents with multiple diagnoses, especially because the level of reimbursement may be tied to the clinical category that encompasses that diagnosis. Understand the Primary Diagnosis Categories While the categories look fairly self-explanatory, it can be hard to figure out the most accurate code. The RAI Manual provides examples of which conditions would fall into each category on pages I-2 to I-3. Note that “medically complex conditions” may include some acute issues, but also chronic conditions that require intensive nursing: “Examples include diabetes, pneumonia, chronic kidney disease, open wounds, pressure ulcer/injury, infection, and disorders of fluid, electrolyte, and acid-base balance,” the RAI Manual says. For fractures and subsequent joint replacements, you can select the ICD-10 code that pertains to the fracture if the resident is admitted to the facility to recover from the injury or resulting operation and receive rehabilitation. Know Stroke Exception Navigating nuance really comes into play if you have a resident who is recovering from stroke, however. The RAI Manual provides a coding example for a resident being transferred to a nursing facility from a hospital, following a stroke, and instructs that the correct ICD-10 code would not be for the stroke itself but for the hemiplegia and hemiparesis that followed. Even though the hypothetical resident had a stroke and the admitting physician listed the stroke as that resident’s main diagnosis, the stroke itself would have been treated in the hospital. The nursing facility won’t be administering medicine to break up a clot or any other emergency stroke treatments — the facility will be providing nursing and rehabilitation to help the resident regain or maintain function post-stroke. Become Comfortable with Key Terms Beyond determining the primary diagnosis, you’ll have to figure out which (if any) other diagnoses to document on the MDS. CMS instructs nurse assessment coordinators to document active diagnoses. It may be tough to figure out what counts as “active” when looking at a medical history including conditions that may still affect a resident’s function or cognition or mobility, even if those medical events happened years ago. Definition: On page I-7, the RAI Manual explains that active diagnoses are: “Physician-documented diagnoses in the last 60 days that have a direct relationship to the resident’s current functional status, cognitive status, mood or behavior, medical treatments, nursing monitoring, or risk of death during the 7-day look-back period.” The RAI Manual explicitly states that nurse assessment coordinators should not include diagnoses that “have been resolved, do not affect the resident’s current status, or do not drive the resident’s plan of care during the 7-day look-back period,” explaining that CMS considers such diagnoses “inactive” for this section on the MDS. Know, too, that determining whether a condition requires “nurse monitoring” can be a means of figuring out if a diagnosis is “active.” The RAI Manual defines nurse monitoring as including all clinical monitoring performed by a licensed nurse. So, for example, when deciding what to code for a resident who had a hip replacement three years ago and hasn’t been independently ambulatory since, you would not select hip fracture as an active diagnosis. Bottom line: Even though many residents’ medical histories and current medical conditions are complicated, try to see through to the black-and-white clinical documentation: which condition caused the resident to be admitted to the facility and which condition(s) require active care or required care in the past seven days. “These situations can be complicated and involved and many times the nurse assessment coordinator will need to query the physician (or physician extenders). Without clear documentation and realizing that the nurse cannot diagnose the key decision will need the input from the physician,” says Jane Belt, Ms, RN, RAC-MT, RAC-MTA, QCP, curriculum development specialist at American Association of Post-Acute Care Nursing (AAPACN). See the You Be The Coder scenario to test whether you have this distinction under your belt.