How Your Coding Affects Bladder/Bowel Long-Stay Quality Measure
Take these 8 steps now to improve your QM score.
The MDS 3.0 quality measure (QM) “Percent of Low Risk Residents Who Lose Control of Their Bowel or Bladder (Long Stay)” draws from your coding of several MDS sections, not just Section H — Bladder and Bowel. And if your score for this measure isn’t so great, you need to first understand why, and then employ expert strategies to beef up your performance. Here’s how.
What Counts Toward This QM
Keep in mind that this is a long-stay measure, which applies to residents who are in your facility for 101 or more cumulative days, according to a recent training by Maureen Valvo, BSN, RN, RAC-CT, senior quality improvement specialist with the Quality Improvement Organization (QIO) IPRO, part of the Atlantic Quality Innovation Network. The cumulative day count does not include days the resident is out of the facility.
Significance: Although this is not one of the QMs in the Five Star Rating, it is used in the Certification and Survey Provider Enhanced Reporting (CASPER) QM Report, Nursing Home Compare, Nursing Home Quality Care Collaborative (NHQCC) Composite Measure Score, and the annual survey process.
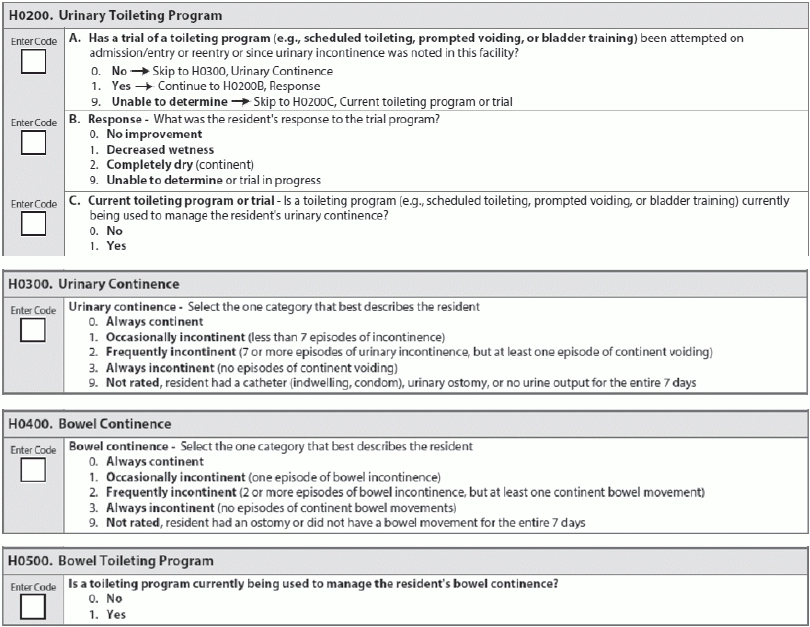
The bowel/bladder QM is calculated primarily from your coding of Items H0300 — Urinary Continence and H0400 — Bowel Continence. The numerator is the number of long-stay residents with a selected target assessment that you’ve coded as 2 — Frequently incontinent or 3 — Always incontinent for H0300 or H0400. Coding 2 or 3 for H0300 or H0400 will trigger this QM, Valvo noted.
You would code 2 for H0300 if, during the seven-day lookback period, the resident was incontinent of urine seven or more episodes but had at least one continent void. For H0400, you would code 2 if, during the lookback period, the resident was incontinent of bowel more than once but had at least one continent bowel movement.
Code 3 for H0300 if the resident had no continent voids during the seven-day lookback period. Code 3 for H0400 if the resident was incontinent of bowel for all bowel movements and had no continent bowel movements.
Then, the denominator is the number of all long-stay residents with a selected target assessment, except those with certain “exclusions.”
Understand 8 Important Exclusions
Purpose: These exclusions prevent certain residents’ assessments from being included in the QM and this is how CASPER determines which residents qualify as “low risk,” according to the Texas Department of Aging and Disability Services (DADS). The exclusions aim to remove from the equation those assessments with conditions for which bowel and/or bladder issues are most common, as well as those assessments where the relevant data items were not assessed (dashed or skipped) and therefore not known.
The specific exclusions are as follows:
1. Target assessment is an admission assessment (A0310A = 01) or a PPS five-day or readmission/return assessment (A0310B = 01, 06).
2. Resident is not in numerator and H0300 = [-] or H0400 = [-].
3. Residents who have any of the following high-risk conditions:
a. Severe cognitive impairment on the target assessment (C1000 = 3 and C0700 = 1) or (C0500 ≤ 7);
4. Resident does not qualify as high risk (see #3 above) and both of the following two conditions are true for the target assessment:
a. (C0500 = 99, [^], [-]), and
5. Resident does not qualify as high risk (see #3 above) and any of the following three conditions are true:
a. (G0110A1 = [-]); or
6. Resident is comatose (B0100 = 1) or comatose status is missing (B0100 = [-]) on the target assessment.
7. Resident has an indwelling catheter (H0100A = 1) or indwelling catheter status is missing (H0100A = [-]) on the target assessment.
8. Resident has an ostomy (H0100C = 1) or ostomy status is missing (H0100C = [-]) on the target assessment.
3 Steps for Assessment of Bladder/Bowel Incontinence
How you code residents’ continence and incontinence plays a key role in the calculations for this QM, so you need to make sure there is no miscoding of Section H on the MDS. This is especially true if you have residents who’ve triggered the bladder/bowel QM but perhaps shouldn’t have.
Your assessment is similar for both bladder and bowel incontinence, Valvo noted. The steps for assessment are:
1. Review residents’ incontinence records, nursing assessments, progress notes, physician history, and physical examination. “Be sure that the system of documentation includes clear identification of continent or incontinent episodes,” Valvo said.
2. Interview the resident if he is capable of reliably reporting continence. Also, talk with the resident’s family members or significant others.
3. Ask the direct care staff who routinely work with the resident on all shifts about incontinence episodes among the residents.
Mistake: One common coding error is “coding a resident as always incontinent even if, during the lookback period, the resident voluntarily urinated once in a potted plant, or was assisted or made it to the toilet once and voided,” DADS noted. Keep in mind that a resident can be incontinent seven, 10, 16 or 25 times during the seven-day lookback period, but one continent void at any time during this timeframe makes the correct coding 2 — Frequently incontinent.
Further, the RAI Manual’s definition of continence indicates that a resident who decides to void in a potted plant, his roommate’s closet, or another resident’s bedside commode is continent, DADS explained. “It may be that these are not appropriate places to void and these behaviors should be addressed in the care plan, but the resident is still coded as continent.”
On the other hand, you cannot dismiss incontinence even if it occurs due to certain factors. For example, if a resident has bowel incontinence due to loose stools or diarrhea from illness, use of laxatives, or any other cause, this would still count as incontinence.
Employ Care Planning & Incontinence Improvement Strategies
That doesn’t mean, however, that you don’t still need to care plan for these factors.
Pay attention: “Provided the assessments were coded correctly, you should also think of this QM as a flag that prompts you to review the toileting needs for those residents that do trigger,” DADS advised. Because the triggering residents are categorized as “low risk,” the care team staff should ask themselves if there are any steps they can take to improve a resident’s incontinence.
When care planning for bladder incontinence, you must assess the type and cause of urinary incontinence, Valvo stressed. “For many residents, incontinence can be resolved or minimized by identifying and treating underlying potentially reversible causes.” (See “Know the Types of Urinary Incontinence for Optimal Care Planning on page 10 for specific types of urinary incontinence.)
Employ incontinence improvement strategies such as eliminating environmental physical barriers to accessing commodes, bedpans, and urinals, as well as obtaining assistance. Also, make sure the care plan includes other strategies as appropriate like bladder retraining, prompted voiding, scheduled toileting, or bowel toileting programs. For bowel incontinence, also consider any potentially reversible causes like medication side effects, constipation and fecal impaction, immobility, and diet.
Overall, your incontinence improvement strategies should include the following:
Caveat: You may have some residents who consistently trigger this QM, because they just miss being included in one of the exclusion categories — for instance, the resident’s BIMS summary is an eight or the resident has some slight ability to assist with transfer, DADS pointed out. “In such cases, all a facility can do is ensure [staff] are coding their assessments correctly and handling the resident’s toileting needs appropriately.”
Action Points: Improve Your Bladder/Bowel QM Score
So, you’ve coded the assessments correctly, but your bladder/bowel QM score isn’t what you’d like it to be. What can you do?
Valvo recommended the following steps as a model for improving your QM score:
1. Analyze the data to determine a root cause and/or quality improvement opportunity, and use concurrent data monitoring as you work through your quality improvement process;
2. Drill down the information to the resident level, and have the interdisciplinary team review and assess the residents who are triggering the QM;
3. Assess the coding accuracy of the MDS for the residents triggering the QM, and ensure that there isn’t an electronic entry error;
4. Verify that the medical record documentation supports the coding in relation to the Assessment Reference Date (ARD);
5. Assess the interviewers’ experience and the effects of flawed interview skills/techniques on the MDS data and QM score specific to evaluating cognitive status and memory;
6. Assess the effect of staff stability/consistent assignment practice with providing resident care, especially for providing assistance, evaluating toileting issues, and identifying toileting needs;
7. Develop individualized care plans focusing on quality improvement closest to the resident; and
8. Measure overall effectiveness of quality improvement interventions.
b. Totally dependent in bed mobility self-performance (G0110A1 = 4, 7, 8);
c. Totally dependent in transfer self-performance (G0110B1 = 4, 7, 8); or
d. Totally dependent in locomotion on unit self-performance (G0110E1 = 4, 7, 8).
b. (C0700 = [^], [-]) or (C1000 = [^], [-]).
b. (G0110B1 = [-]); or
c. (G0110E1 = [-]).