Official Guidance: Finally, CMS Gives You Clarification On Entry/Reentry Coding
‘Reentry’ definition gets a makeover, A1600–A1900 coding tips get revamped.
After months of confusion and frustration over various Section A coding changes in the MDS 3.0 and RAI Manual instructions, you at long last have the explanations you’ve been searching for.
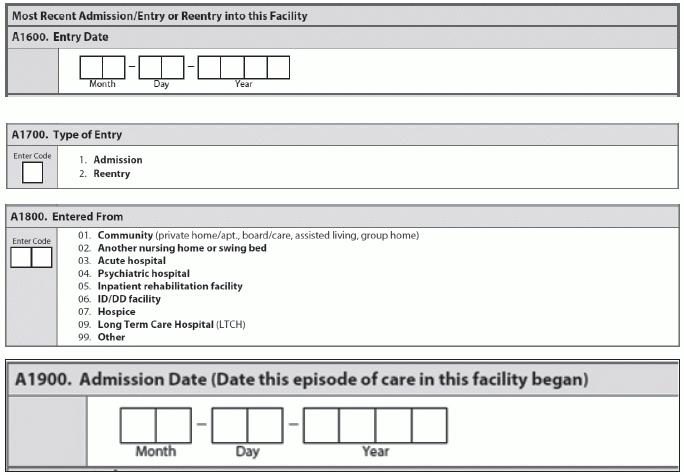
On Feb. 5, the Centers for Medicare & Medicaid Services (CMS) released a new errata document with additional revisions to the MDS 3.0 RAI Manual v1.12R. The revisions clarify the meaning of entry/reentry and explain the correct coding for items A1600 — Entry Date, A1700 — Type of Entry, A1800 — Entered From, and A1900 — Admission Date. All the newly revised pages in the RAI Manual bear the footer “October 2014 (R)” or “October 2014 (R2).”
How Definition of ‘Reentry’ Has Changed
First, in Chapter 2, page 2-13 (under 2.5), “Assessment Types and Definitions,” CMS revised the definition of “reentry.” The definition now reads as follows:
“Reentry refers to the situation when all three of the following occurred prior to this entry: the resident was previously in this facility and was discharged return anticipated and returned within 30 days of discharge. Upon the resident’s return to the facility, the facility is required to complete an Entry tracking record. In determining if the resident returned to the facility within 30 days, the day of discharge from the facility is not counted in the 30 days. For example, a resident who is discharged return anticipated on December 1 would need to return to the facility by December 31 to meet the ‘within 30 days’ requirement.”
Consider 3 Events When an Episode Continues Across Stays
Then, in Section A of Chapter 3, on page A-26, CMS completely revamped the “Coding Tips and Special Populations” section for items A1600 through A1900. The RAI Manual indicates that both swing bed facilities and nursing homes must use these instructions for coding items A1600 through A1900 to determine whether a resident is an admission/entry or reentry.
CMS specified that the new item A1900 — Admission Date is tied to items A1600 — Entry Date, A1700 — Type of Entry, and A1800 — Entered From. A1900 is also tied to the concepts of a “stay” and an “episode.” A stay is a set of contiguous days in the facility, while an episode is a series of one or more stays that may be separated by brief interruptions in the resident’s time in the facility.
Pay attention: An episode would continue across stays until one of three events occurs:
1. The resident is discharged with return not anticipated; OR
Important: The Admission Date in A1900 should remain the same on all assessments for a given episode and should change only when a new episode begins. The Entry Date in A1600, however, would change whenever a new stay begins. So when a resident is discharged and reenters within the course of an episode, the date in A1600 would change but the date in A1900 would remain the same.
Understand Coding Differences Among Separate Stays
Upon a resident’s first admission to your facility, you must code the Entry Date in A1600 as the date the resident first entered your facility. Code the Type of Entry in A1700 as 1 — Admission, and then document the place from where the resident came in item A1800. The Admission Date in A1900 should match the Entry Date in A1600.
You should code these items the same way for all subsequent assessments within the first stay of an episode.
Caveat: If the resident is briefly discharged and then reenters your facility, a new (second) stay would begin, but the current episode would continue. On the Entry Tracking Record and on subsequent assessments for the second stay, the Entry Date in A1600 would change depending on the date of reentry.
Also, you would code the Type of Entry in A1700 as 2 — Reentry, and then code Entered From in A1800 to reflect where the resident was prior to this reentry. But unlike A1600, the Admission Date in A1900 would continue to show the original admission date, the start date of the first stay in this episode.
Bottom Line: Follow 3 ‘Golden Rules’ When Coding Entry/Reentry
Rule 1: When determining whether a resident returned to your facility within 30 days, keep in mind that you do not count the day of discharge from your facility in the 30 days. For example, when a resident is discharged return anticipated on Dec. 1, he would need to return to your facility by Dec. 31 to meet the “within 30 days” requirement.
Rule 2: If you code A1700 — Type of Entry for an assessment as 1 — Admission, items A1900 — Admission Date and A1600 — Entry Date must be the same.
Rule 3: If you code A1700 as 2 — Reentry for an assessment, item A1900 will remain the same, and the Entry Date in A1600 must be later than the date in A1900.
Look for OBRA Admission Assessment Revisions
Coinciding with the various entry/reentry revisions, CMS also made changes to several parts of Chapter 2 that deal with OBRA Admission assessments. Here are the revisions:
The Admission definition now indicates that completion of an OBRA Admission assessment must occur in any of the following admission situations:
o When the resident has never been admitted to this facility before; OR
The “01. Admission Assessment (A0310A=01)” requirements now indicate that you must complete an Admission assessment for a new resident and, under some circumstances, a returning resident by the end of Day 14, counting the date of admission as Day 1 if:
o This is the resident’s first time in this facility; OR
Check Out Other Manual Changes
Finally, CMS made a few other minor tweaks and corrections to Chapter 2 and Section A of Chapter 3:
1. Mr. W. was admitted to the nursing home on April 11, 2011. Four weeks later he became very short of breath during lunch. The nurse assessed him and noted his lung sounds were not clear. His breathing became very labored. He was discharged return anticipated and admitted to the hospital on May 9, 2011. On May 18, 2011, Mr. W. returned to the facility. Code the Entry tracking record for the May 18, 2011 return as follows:
A0310F = 01
Code the Item A0310 of the MDS 3.0 as follows:
A0310A = 99
Resource: To access the new errata document, go to www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/Downloads/MDS-3-RAI-Manual-v-1-1-2-R-Errata.pdf. Or you can visit www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/MDS30RAIManual.html and access the errata document and change tables by scrolling down to the links in the Downloads section at the bottom of the webpage.
2. The resident is discharged with return anticipated but is out of the facility for more than 30 days; OR
3. The resident dies in the facility.
o When the resident has been in this facility previously and was discharged return not anticipated; OR
o When the resident has been in this facility previously and was discharged return anticipated and did not return within 30 days of discharge.
o The resident has been admitted to this facility and was discharged return not anticipated; OR
o The resident has been admitted to this facility and was discharged return anticipated and did not return within 30 days of discharge.
A1600 = 05-18-2011
A1700 = 2
A0310B = 01, 02, 03, 04, or 05 as appropriate
A0310C = 1
A0310D = 0 (Swing Beds only)