Clear Up Your Coding Confusion Over New Item A1900
Strategy: Understand when the episode of care does or does not end.
If you’re struggling with correctly coding A1900, you’re not alone. Although the Centers for Medicare & Medicaid Services (CMS) added this new item in the October 2014 RAI Manual update, you didn’t get a full explanation on how to code A1900 properly.
What ‘Stay’ and ‘Episode of Care’ Mean for Section A Items
Specifically for A1900 — Admission Date (Date this episode of care in this facility began), the RAI Manual does not thoroughly explain the meaning of “episode of care” or of a “stay.”
Definition: “A stay is a set of contiguous days in the facility and an episode is a series of one or more stays that may be separated by brief interruptions in the resident’s time in the facility,” explained Judy Bennett, CPA, MDS Automation Coordinator for the Washington State Department of Social and Health Services’ Aging and Long-Term Support Administration, in a recent ListServ posting.
An episode continues across stays until one of three events occurs:
1. The resident is discharged with return not anticipated;
Which Items Work in Tandem with A1900
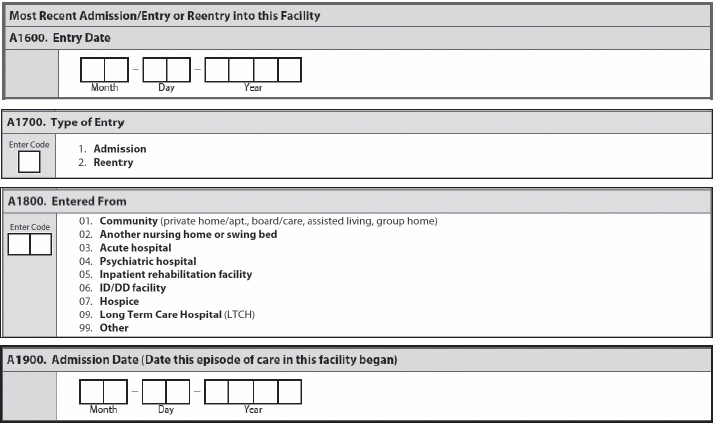
A1900 affects three other items in the MDS: A1600 — Entry Date; A1700 — Type of Entry; and A1800 — Entered From. When the resident first comes to your facility, the dates for A1600 and A1900 will be the same on the Entry tracker, stated the Pennsylvania Department of Health’s (PADH) November 2014 RAI Spotlight. “It is the beginning of both the episode and the stay.”
Also when the resident is first admitted to your facility, you would code A1700 as 1 — Admission and A1800 as the most recent “entered from” location before admission, Bennett explained. “These items would be coded the same way for all subsequent records within that first stay within the episode.”
“The admission date should remain the same on all assessments for a given episode, even if it is interrupted by temporary discharges from the facility,” Bennett continued. “If the resident is discharged and reenters within the course of the episode, that will start a new stay. The most recent entry date will change, but the admission date will remain the same.”
Bottom line: This means that all records for a given stay will have the same entry date, and the admission date in A1900 will remain the same for all records within the episode.
Code This Way When Resident Leaves Briefly
But if the resident is returning from a period of hospitalization, you would code A1600 as the latest date of reentry, PADH said. The date for A1900 would not change.
“The episode doesn’t end until the resident is Discharged Return Not Anticipated, Discharged Return Anticipated but stays out more than 30 days, or dies,” PADH explained.
In this case, the resident’s reentry into the facility would start a new, second stay but would continue the episode, Bennett clarified. Although the admission date in A1900 would continue to show the resident’s original admission date (the date that began his first stay), on the Entry tracking record and on subsequent assessments for the second stay, the type of most recent entry for Item A1700 would be 2 — Reentry.
And you would code the most recent entry date in A1600 as the day the resident reentered the facility for the second stay. The most recent “entered from” location in A1800 is the location before this reentry. And this coding would be the same for any subsequent stays within that episode.
“The episode would end if the resident had a discharge return not anticipated or if there was a gap of more than 30 days out of the facility,” Bennett noted. “If the resident returned to the facility after such an event, then a new episode would begin and would be coded as a new admission.”
Admission Vs. Reentry: What You Need to Know
Although the OBRA Admission assessment requirements have not changed, certain changes that were effective on Oct. 1 have impacted your coding.
Old way: Before Oct. 1, if a resident was discharged prior to Day 14 and returned, you would complete an Entry tracking record and code A1700 as 1 — Admission, noted Jill Sumner, vice president of health policy and integrated services advocacy for Washington, D.C.-based Leading Age, in a Dec. 8 analysis.
New way: Now the presence or absence of the OBRA Admission assessment is not relevant to the type of Entry tracking record you completed, Sumner explained. You would code Item A1700 as 1 — Admission every time a resident:
You would code A1700 as 2 — Reentry every time a resident:
Example: Mrs. Jones was not in a Medicare Part A skilled nursing facility (SNF) stay and was admitted on Feb. 4, 2015. She was emergently discharged to the hospital on Feb. 9 and was readmitted on Feb. 15, and then she remained in the facility long-term.
According to Sumner, you would need to complete the following required assessments:
According to Sumner, if Mrs. Jones was in a Medicare Part A SNF stay, you would complete the following required assessments:
2. The resident is discharged with return anticipated but is out of the facility for more than 30 days; or
3. The resident dies in the facility.