Don’t Fall Prey to COVID-19 Cyberattacks
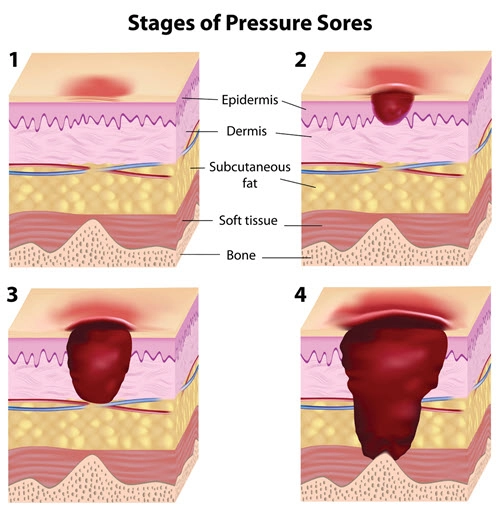
Question: Which ICD-10 code should I choose for a resident who has two stage 2 pressure injuries, aka pressure ulcers or pressure sores, on the right buttock? Should I use the same diagnosis code twice, as the guidelines for the Diseases of the Skin and Subcutaneous Tissue chapter direct me to, or should I only use the same code once as it could look like an accidental code duplication? North Dakota Subscriber Answer: While you are correct in saying ICD-10 guidelines require you to “assign as many codes from category L89 as needed to identify all the pressure ulcers the patient has, if applicable” (1.C.12.a.1), in this case, doing so could create unnecessary confusion and, quite possibly, a claim submission error. Had the ulcers been in separate locations, or of different stages, two codes would have been needed, and you would put the most severe first, assuming your provider was treating both at the same time. However, in this encounter, both ulcers are of the same severity and location, so you would use L89.312 (Pressure ulcer of right buttock, stage 2) only once to document this patient’s condition.