Palliative Care Isn't Always Hospice Care
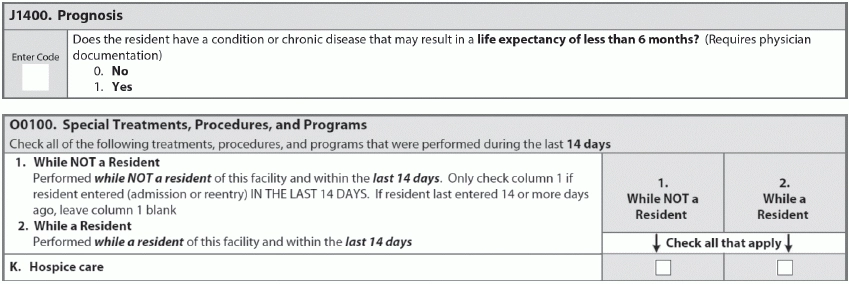
Question: My colleague and I disagree about whether palliative care automatically equals hospice care. Do I record a resident as being on hospice if she’s receiving palliative care provided by our facility? Texas Subscriber Answer: Hospice and palliative care are different. The Resident Assessment Instrument (RAI) Manual, on page O-5, says: “Code residents identified as being in a hospice program for terminally ill persons where an array of services is provided for the palliation and management of terminal illness and related conditions. The hospice must be licensed by the state as a hospice provider and/or certified under the Medicare program as a hospice provider.” So, while a resident may be receiving palliative care, remember: If she’s not being cared for by a licensed or Medicare-certified hospice program, then she’s technically not on hospice and you should not code her condition as such. So, with the information you provided, and with the understanding that the resident is not on hospice and wasn’t on hospice at any point in the past 14 days, you should not check either box 1 or 2 for item O0100K (Special Treatments, Procedures, and Programs Hospice care). However, if your facility is administering palliative care with the understanding on a physician’s orders, with the understanding that the resident is dying, make sure you don’t forget to code J1400 (Prognosis).