Quality:
Which Measures Can You See On Your CASPER QM Reports?
When you’re dealing with quality measures (QMs) that will impact your reimbursement, you need to be proactive instead of reactive. You can keep your eyes on your quality scores by accessing your QM reports through the Center for Medicare & Medicaid Services’ (CMS) CASPER reporting system.
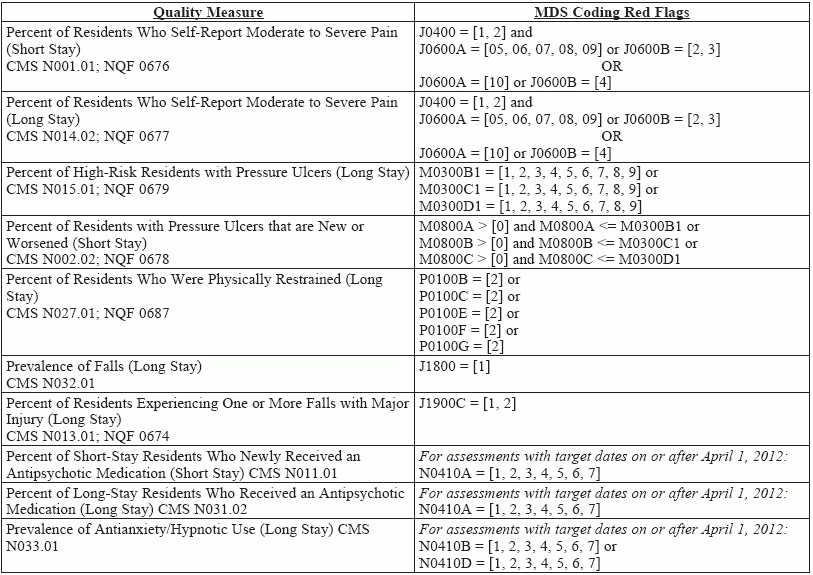
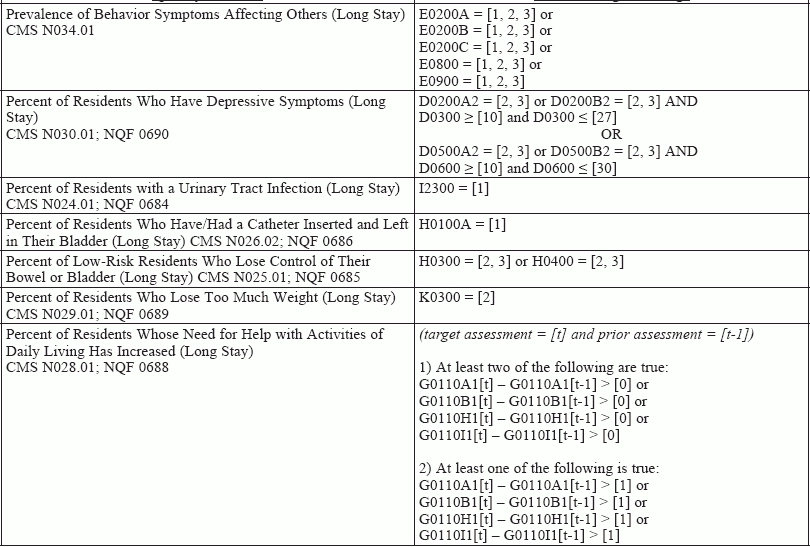
The CASPER reports contain a subset of the main QMs, plus several additional measures that are available only on the CASPER reports. Use this table to learn which QMs are available to you on the CASPER reports — and which MDS 3.0 items will contribute to those measures when you code them in specific ways.