MDS Alert
Take 6 Steps Now To Improve Your Behavior QM Score
Consider these additional factors when a resident is wandering.
The Centers for Medicare & Medicaid services (CMS) is pushing hard for nursing facilities to eliminate the use of antipsychotic medications in residents with dementia. But as you take your residents off these types of meds, you might find your staff dealing with increasing behavior issues in dementia patients — and this could have a negative impact on one of your surveyor quality measures (QMs).
Specifically, medication changes may impact your score for the surveyor QM “Prevalence of Behavior Symptoms Affecting Others.” This is a long-stay measure, and residents who trigger it tend to have a dementia diagnosis, according to a recent blog posting by Kathy Monahan for Harmony Healthcare International.
Understand Which Residents Will End Up in the QM
This surveyor QM reports the percentage of long-stay residents who have behavior symptoms that affect others during the seven-day look-back period. This QM is one of three QMs for surveyors and are available to State Surveyors and nursing facilities only through the CASPER Reporting System, according to the New England Quality Innovative Network (NEQIN).
This QM aims to identify behavioral symptoms that may be distressing or disruptive to residents, staff members or the care environment, according to CMS. “These behaviors may place the resident at risk for injury, isolation and inactivity, and may also indicate unrecognized needs, preferences or illness.”
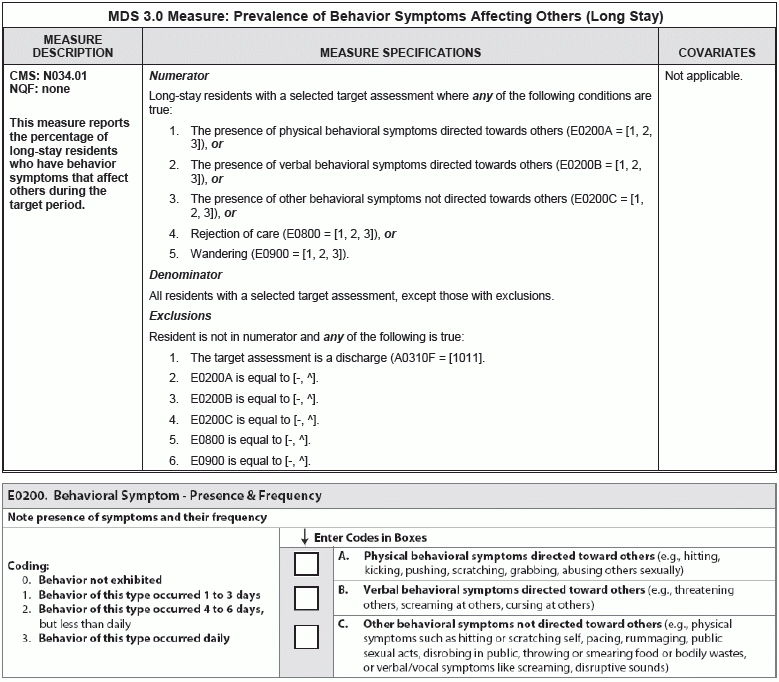
Pay attention: The behaviors affecting others QM captures all long-stay residents with the following specific conditions coded on their target MDS assessment as 1 — Behavior of this type occurred 1 to 3 days, 2 — Behavior of this type occurred 4 to 6 days but less than daily, or 3 — Behavior of this type occurred daily:
- E0200A — Physical behavioral symptoms directed toward others;
- E0200B — Verbal behavioral symptoms directed toward others;
- E0200C — Other behavioral symptoms not directed toward others;
- E0800 — Rejection of Care – Presence & Frequency; or
- E0900 — Wandering – Presence & Frequency.
A resident will trigger the QM on the MDS 3.0 Facility Level QM Report if the most recent MDS (the target assessment) has any one of the above conditions coded, the NEQIN states. These are included in the numerator. Note that this QM has no covariates.
The denominator includes all long-stay residents with a selected target assessment, except for those with a specific exclusion. A resident is excluded if the resident is not in the numerator and any of the following is true:
- The target assessment is a discharge assessment, A0310F — Entry/discharge reporting is coded as 10 — Discharge assessment-return not anticipated or 11 — Discharge assessment-return anticipated; OR
- E0200A, E0200B, E0200C, E0800 or E0900 is coded with a dash [-].
Follow 6 Tips to Ace This QM
If you have a significant number of residents who trigger this QM, you can take some specific actions to reduce this number and improve your quality score for this measure. Monahan provides the following steps:
1. Create an Action Team: You should develop an “Action Team” that consists of direct care staff, nursing and rehab leadership, physicians and nurse practitioners, activities staff, and pharmacists.
2. Develop an assessment process: Ensure that speech and occupational therapy staff have identified the stage of dementia in which each resident is functioning. The Global Deterioration Scale and Allen Cognitive Assessments can identify clinical characteristics of dementia, and the Allen Assessment identifies if the resident has any new learning ability and identifies patient strengths.
Then, you can develop care plans and teaching programs for staff based on the results of the assessments. These can help staff with managing behaviors, as well as using appropriate approaches and cueing strategies to reduce behavior triggers.
3. Detect any sensory component of the behaviors: Encourage your therapists to play a lead role in assessing each resident’s sensory and neurological processing to determine if there is a sensory component of the behaviors. Environmental stimuli like room temperature, noises, lights, and even clothing can all trigger behavior reactions in residents with dementia.
Therapists can develop “sensory diets” involving sensory activities designed to calm agitated residents, stimulate somnolent residents, and assist residents in maintaining control of their emotions during Activities of Daily Living (ADLs) or meals, Monahan noted.
4. employ your activities department and social services: Also, you can encourage your activities department to design social activities for residents while grouped together by their cognitive levels. Social services can assess residents upon admission to identify past history and interests, and then share this information with the Action Team and incorporate the activities into the facility programming.
5. Set up the care plan: Have each discipline set up a care plan, goals, and interventions based on the resident’s dementia level and functional level.
6. Utilize therapy sensory assessments: You can also use therapy sensory assessments to analyze the resident’s behaviors. Residents with dementia may often display behaviors as the result of an unmet need, so the key to managing the behaviors is to identify what that need is.
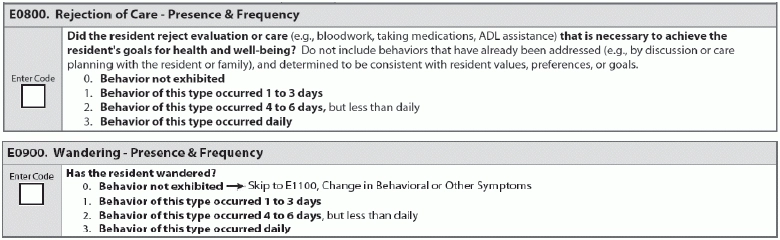
For wandering, you should assess the resident for the underlying reason, and determine the frequency and any factors that trigger the behavior or that decrease the episodes of wandering, the RAI Manual advises. Make sure that you assess for the following underlying reasons that may be contributing to wandering:
- Tension;
- Anxiety;
- Psychosis;
- Drug-induced psychomotor restlessness;
- Agitation; and/or
- Unmet need (e.g., food, fluids, toileting, exercise, pain relief, sensory or cognitive stimulation, sense of security, companionship).
Resources: To access this and other surveyor QMs, go to www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/nursinghomequalityinits/nhqiqualitymeasures.html. And the latest Technical User’s Guide for the Five Star Nursing Home Quality Rating System is available at www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/nursinghomequalityinits/nhqiqualitymeasures.html.
MDS Alert
- Quality Measures:
Take 6 Steps Now To Improve Your Behavior QM Score
Consider these additional factors when a resident is wandering. The Centers for Medicare & Medicaid [...] - Compliance:
What To Expect From The Second Round Of RoP Challenges
Heads up: PRN orders for these medications are now limited to 14 days. If your [...] - Regulations:
Take Control Of Your RoP Compliance With This Phase 2 Checklist
Make sure you stay on top of all the new programs, forms, and systems. Phase [...] - Quiz:
Test Your Skills For Coding The Pain Assessment Interview
Are rates of self-reported pain higher or lower than those of observed rates? Being able [...] - What Would You Do?
Question 1: Why do my correction/modifications get rejected? Answer 1: If the ASAP system rejects [...] - Section O:
Study 7 Scenarios To Hone Your Restorative-Nursing Coding
Don’t make this mistake when you should actually code 0. Incorrectly coding item O0500 — [...] - Answer Key:
Pain Assessment Interview
Answer 1: c) 5 days. The look-back period for items J0300 through J0600 is five [...]

