Leave Restraints Behind: Go Beyond Coding on Section P
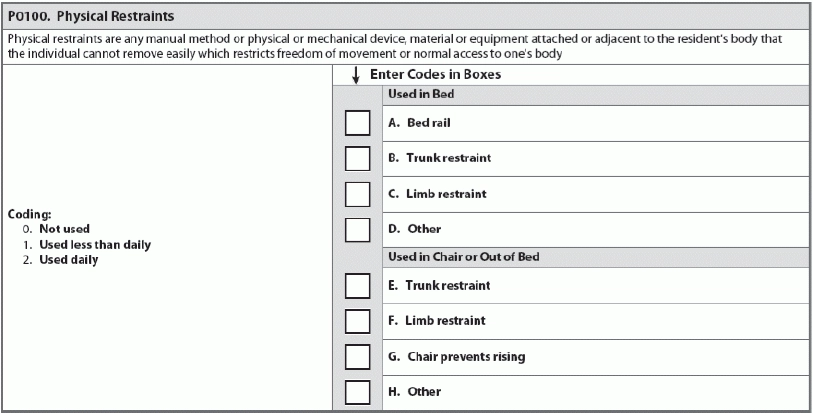
The definition of ‘restraint’ keeps evolving. Section P seems straightforward, with only nine options to code whether restraints were used while a resident was in bed or out of bed, and if used, which parts of the body were restrained. But you may be surprised at what the MDS considers a restraint, both now and in the coming update. The MDS defines a restraint as “any manual method, physical or mechanical device, material or equipment attached or adjacent to the resident’s body that the individual cannot remove easily, which restricts freedom of movement or normal access to one’s body.” Caution: Surveyors can give F-tags (F221, F222) for physical or chemical restraints applied for “purposes of discipline or convenience and not required to treat the resident’s medical symptoms.” Tricky: Surveyors may consider even the most innocuous seeming items as restraints. Any object staff places on a resident that she cannot remove independently and easily could qualify as a restraint. Example: Ms. Rosenstein hates having her nails trimmed — she has always maintained long nails — and sometimes accidentally scratches herself or a staff member. A team member suggested that Ms. Rosenstein wear mittens overnight and while she gets out of bed, when the majority of accidental scratching incidences occur. In this situation, the mittens could qualify as a limb restraint used daily in in bed and in chair or out of bed per PO100 (physical restraints). Similarly, bedrails, which can serve a crucial safety function, can also function as an unnecessary restraint, depending on the particular resident and medical symptoms. Bedrails, also referred to as side rails, can be dangerous if residents are mobile enough to try to exit the bed without assistance. Residents are at risk of injury or death if they try to exit the bed through or around the bedrails; residents are at even greater risk of serious injury if they try to exit a bed with raised side rails and fall versus a bed without raised side rails. It’s also important to think about bedrails as a less obvious form of restraint: Residents might spend more time in bed because the bedrails prevent them from exiting the bed without assistance. Choosing to use bedrails, and using them effectively and safely, is a matter of assessing each individual resident’s condition and mobility, even from week to week. What qualifies: If you, a team member, a family member, or a surveyor could look at an object being used by the resident and define it as a restraint, make sure the restraint is documented accordingly, per the RAI Manual: This kind of comprehensive documentation is crucial for both staff intent and the effect on residents, and will go a long way in preventing F-tags, but team members should carefully evaluate restraint use for resident safety, happiness, and facility policy. The RAI manual notes: “While a restraint-free environment is not a federal requirement, the use of physical restraints should be the exception, not the rule.” CMS guidelines encourage reducing the use of restraints, as many negative outcomes are associated with their implementation. Consider this Case Study for Context The following case study is from Senior Advocacy Services Ombudsman Program HICAP: Problem: When the ombudsman visited a skilled nursing facility, she found Fred confined in his wheelchair with a belt wrapped around him. Fred appeared to be agitated that he could not remove the belt. Action: The ombudsman asked Fred if he could unfasten the belt, and he clearly could not. The nurse said he had to have the belt on so he wouldn’t fall, and said there was a doctor’s order for the restraint for safety. The ombudsman quoted the regulations that stated that a restraint could not be used unless the resident could personally unfasten the belt. The belt can only be used for a stated length of time while a medication change gets under control, or for mobility purposes, but it cannot be used to restrain a person in the chair. The nurse did not remove the belt. The ombudsman filed a complaint with licensing. Outcome: Licensing made a visit to the nursing home and cited the facility for improper use of a belt. The doctor re-wrote the order for the belt to be used for a specified time (under 90 days) until the resident was stabilized with his new medication. Don’t Forget: The next update of the MDS will reflect a big change in the title and usage of Section P, which will incorporate alarms as well as clarification on chemical restraints. Please see MDS Alert, Vol. 15, No. 2, page 14 for more on this update.