O0100: Don't Make These 6 Common Mistakes
Tip: Capture all items, regardless of where the resident received the services.
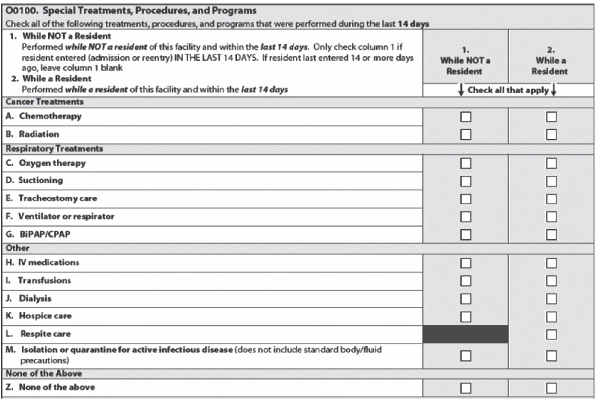
Understanding the finer points of coding O0100: Special Treatments, Procedures, and Programs secures both your facility’s care planning and its reimbursement. Here are the most common mistakes made when coding items under O0100 — and how to avoid them so you can capture all appropriate items.
Don’t Code Services Provided Solely in Conjunction with Surgery
Mistake #1: If the service was provided solely in conjunction with a surgical procedure, do not code it under O0100, according to an instructional seminar by Patsy Strouse, RN, the RAI Coordinator for the Ohio Department of Health.
“If it was during the surgical procedure, or during routine pre- and post-operative procedures, you would not capture it,” Rena Shephard, president of RRS Healthcare Consulting Services in San Diego, CA and a member of the MDS 3.0 development team, said in a Centers for Medicare & Medicaid Services (CMS) presentation.
Example: If the patient was receiving IV antibiotics after surgery because she actually had an infection, you’re going to be able to capture that. But if the patient is getting IV antibiotics in the recovery room for prophylactic purposes only, that’s just routine and you would not code that, Shephard said.
Capture Everything Within the 14-Day Look-Back Period
Mistake #2: The resident does not need to have received the treatment in your facility for you to code it under O0100, as long as he was a resident of your facility, Shephard noted.
“You do capture these treatments and procedures that are listed here in O0100A through M, regardless of where the resident was when he or she received it … as long as it fell into the look-back period for the assessment,” Shephard stated. “You do capture it — it’s just a question of which column do you put it in.”
Check the Correct Column
Mistake #3: If you’re checking items in the wrong columns, you’re affecting your facility’s reimbursement. Why? “Because if you check ‘While a resident,’ then it can contribute to your reimbursement, and if you check ‘While NOT a resident,’ then it doesn’t,” Shephard said.
Use Column 1 if treatments, programs or procedures were received or performed by the resident prior to admission/re-entry, Strouse instructed. Use Column 2 if treatments, programs or procedures were received or performed by the resident after admission/re-entry to the nursing home.
In other words: Column 1 is for “services that were received before the resident was a resident of the facility and it was captured in the look-back period,” Shephard said. “Or sometimes it happens that the resident is a resident of your facility and he’s actually discharged, and then he comes back again and you actually end up capturing that — the time that he was not a resident in your look-back period. So that would go in Column 1 as well.”
Understand What to Capture for Chemotherapy
Mistake #4: Unlike other MDS sections that instruct you to “code according to the classification of the drug and not its use,” under O0100A you should code only those drugs that the resident is receiving to treat his cancer, Shephard said.
In O0100A, you would code any type of chemotherapy agent given as an antineoplastic. “The drugs coded here are used to treat cancer, not for other reasons,” Strouse cautioned.
Another pitfall: Also, you cannot also code any IVs or IV medications and blood transfusions provided during chemotherapy under MDS items K0500A, O0100H and O0100I, Strouse said.
How to Correctly Capture BiPAP/CPAP
Mistake #5: You don’t need to wonder whether you should capture BiPAP/CPAP as “ventilator or respirator” (and that has always been wrong under MDS 2.0), because BiPAP/CPAP are actually on the list under O0100.
O0100C includes continuous or intermittent oxygen therapy to relieve hypoxia. If BiPAP/CPAP is hooked up to oxygen, this is okay to code here, Strouse explained. But do not code hyperbaric oxygen for wound therapy under O0100C.
Tip: If a ventilator or respirator is used as a substitute for BiPAP or CPAP, you can code this under O0100G, Strouse said.
What ‘IV Medication’ Really Means
Mistake #6: You should now know where to capture contrast material, but don’t try to capture every possible fluid that flows through the resident’s IV under O0100H.
“Code any drug or biological (e.g., contrast material) given by IV push, epidural pump, or drip through a central or peripheral port,” Strouse instructed. You can also include under O0100H intrathecal and baclofen pumps, but you cannot include subcutaneous pumps.
“Subcutaneous pumps are not IV,” Shephard agreed. Nor can you capture IV fluids without medications, because this does not constitute “IV medications.” And you cannot capture medications administered during dialysis or chemotherapy either. IV medications that are administered during dialysis or chemo “are considered to be part of that procedure, and so they are not captured here,” she noted.
Remember: Under MDS 2.0, you didn’t capture contrast material, but with MDS 3.0, you can now capture it, Shephard said.