Navigate Hospice Assessments Better with These Tips
Understand which SCSA pathways are necessary. You may know that a Significant Change in Status Assessment (SCSA) is needed when a resident enters hospice care, but what about if a resident is removed from hospice? “It is required to complete a SCSA when a resident enrolls, disenrolls, or changes hospice providers,” says Scott Heichel RN, CIC, RAC-MT, DNS-CT, RAC-CT, director of clinical reimbursement at LeaderStat in Powell, Ohio. Understand What Constitutes Significant Change Three conditions must be met to establish a significant change and trigger the status assessment, according to the RAI Manual on page 2-22: “A ‘significant change’ is a major decline or improvement in a resident’s status that: 1. “Will not normally resolve itself without intervention by staff or by implementing standard disease-related clinical interventions, the decline is not considered ‘self- limiting; Beware: You can’t use an SCSA as a correction to a mistake, such as miscoding on the MDS. “A significant change differs from a significant error because it reflects an actual significant change in the resident’s health status and NOT incorrect coding of the MDS. “A significant change may require referral for Level II Resident Review Evaluations who may or may not have previously been identified by a Preadmission Screening and Resident Review (PASRR) evaluation if a mental illness, intellectual disability (ID), or related condition is present or is suspected to be present.” Look to Date of Hospice Election A resident entering hospice or leaving hospice would qualify for a significant change in status and thus trigger an SCSA. But other special conditions apply, according to the RAI Manual, which you can find on pages 2-23 to 2-24. It will depend on the Assessment Reference Date (ARD), which you can adjust in certain situations. Enrolling in hospice doesn’t always signify a change of status, such as when the resident arrives having chosen hospice. “If a resident is admitted on the hospice benefit (i.e., the resident is coming into the facility having already elected hospice), or elects hospice on or prior to the ARD of the Admission assessment, the facility should complete the Admission assessment, checking the Hospice Care item, O0100K. Completing an Admission assessment followed by a SCSA is not required,” the RAI Manual says. “Where hospice election occurs after the Admission assessment ARD but prior to its completion, facilities may choose to adjust the ARD to the date of hospice election so that only the Admission assessment is required. In such situations, an SCSA is not required. If a resident disenrolls in a hospice program, an SCSA is required. “A SCSA is required to be performed when a resident is receiving hospice services and then decides to discontinue those services (known as revoking of hospice care). The ARD must be within 14 days from one of the following: 1) the effective date of the hospice election revocation (which can be the same or later than the date of the hospice election revocation statement, but not earlier than); The situation gets a bit trickier if the resident disenrolls from hospice after coming into the facility on hospice, but you can remedy it by adjusting the ARD as noted in the RAI manual: “If a resident is admitted on the hospice benefit but decides to discontinue it prior to the ARD of the Admission assessment, the facility should complete the Admission assessment, checking the Hospice Care item, O0100K. Completing an Admission assessment followed by a SCSA is not required. Where hospice revocation occurs after the Admission assessment ARD but prior to its completion, facilities may choose to adjust the ARD to the date of hospice revocation so that only the Admission assessment is required. In such situations, an SCSA is not required.” Caveat: Beware of using “hospice” and “palliative care” interchangeably. Hospice triggers a significant change, and an SCSA is a requirement, but palliative care, which does not have a designated spot on the MDS, does not necessarily trigger an SCSA, says Jane Belt MS, RN, RAC-MT, QCP, curriculum development specialist at American Association of Nurse Assessment Coordination (AANAC) in Denver, and consulting editor for MDS Alert. Editor’s note: The RAI Manual uses both “an SCSA” and “a SCSA.”
2. “Impacts more than one area of the resident’s health status; and
3. “Requires interdisciplinary review and/or revision of the care plan.”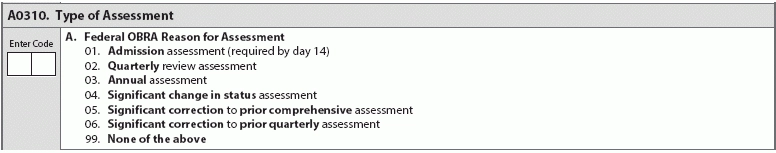
2) the expiration date of the certification of terminal illness; or
3) the date of the physician’s or medical director’s order stating the resident is no longer terminally ill.”

