When you can — and can’t — report medications in J0100.
What should you do if you didn’t have time to complete resident interviews before the Assessment Reference Date (ARD)? How can you figure out whether a diagnosis is “active” and reportable in Section I? Get the answers to these questions and more, straight from the top experts.
CMS gurus tackled some tough MDS questions in the recent American Association of Nurse Assessment Coordinators (AANAC) conference in Las Vegas. Here are a few of the questions and answers:
What if You Didn’t Complete Resident Interviews Before the ARD?
Question 1: If nursing home staff do not complete the interviews before the ARD, how should we code the gateway questions, and should we dash the resident interview items and complete the staff assessments? Or should we insert dashes for both the resident interview and the staff assessment?
Answer 1: You should enter a dash (-) anytime an item is not assessed, answered Jennifer Pettis, RN, BS, WCC, consultant for the Centers for Medicare & Medicaid Services (CMS) Division of Nursing Homes. And you can enter a dash value for nearly all MDS 3.0 items.
Pitfall: But don’t perform a staff assessment just because you didn’t have time to complete the resident interview before the ARD. “There is no information in the RAI User’s Manual that supports completing the staff assessment when the resident interview should be conducted but the staff was unable to do so before the ARD,” Pettis stressed.
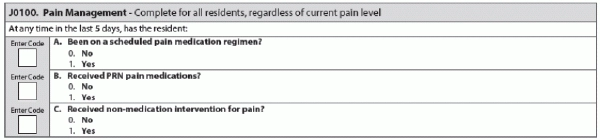
Is This Medication Reportable Under J0100?
Question 2: How can we evaluate a medication for inclusion in J0100 — Pain Management? If we order a medication specifically to treat pain, but the medication is primarily classified for another condition, would we still count this medication here?
Answer 2: Yes, you would include all medications used for pain management purposes, even if the drugs aren’t labeled that way specifically. The only caveat is a medication the resident is using primarily for a condition other than pain that may also provide pain relief. Pettis pointed to the RAI Manual’s definition of a pain medication regime (page J-1):
“Pharmacological agent(s) prescribed to relieve or prevent the recurrence of pain. Include all medications used for pain management by any route and any frequency during the look-back period. Include oral, transcutaneous, subcutaneous, intramuscular, rectal, intravenous injections, or intraspinal delivery. This item does not include medications that primarily target treatment of the underlying condition, such as chemotherapy or steroids, although such treatments may lead to pain reduction.”
What to Consider When Reporting Active Diagnoses
Question 3: Would depression be considered an active diagnosis in Section I in the following example? A resident has a diagnosis of depression in the last 60 days and is treated daily with Trazadone, with no psychiatric monitoring during the seven-day look-back period, no depressive symptoms during the look-back, and normal standard of care nursing monitoring of medication administration.
The resident does have a care plan for depression in place with a goal of being free from depressive symptoms while receiving the lowest therapeutic doses of psychotropic medications. The resident’s daughter has communicated her father’s long history of depression to nursing home staff, and we’ve obtained the resident’s history from the psychiatrist.
Answer 3: Because your facility’s physician documented the diagnosis of depression within the last 60 days, you’ve met the first qualifier for coding I5800 — Depression (other than bipolar), Pettis answered. And you’ve met the second qualifier (the diagnosis is considered active), because:
Also: Make sure that there is monitoring of the Trazadone’s efficacy in the care plan, not just a note about depression being a problem.