Know which organs are involved to narrow down choices.
Urinary tract infections (UTIs) are commonplace in nursing facilities, but do you know whether a UTI is a reason for a resident to enter a nursing facility and for the facility to receive payment for providing care? Find out.
Note that some diagnosis codes are “Return to Provider” but others map into various Patient-Driven Payment Model clinical categories.
Tip 1: Focus on Associated Symptoms
Starting point: The first ICD-10-CM code that pops up when you search for “infection/urinary (tract)” is N39.0 (Urinary tract infection, site not specified). But when you dig further into the listing, you’ll find codes for UTIs that are associated with conditions such as pregnancy or childbirth. You’ll also find entries for different organs and anatomic locations where a “urinary” infection might strike: the bladder, kidneys, and urethra.
Because there are a number of symptoms that might point to UTI but aren’t UTIs themselves, you’ll want to consider every symptom that the physician documented. Some signs and symptoms are consistent with a UTI, such as:
Documentation might also show that the resident has a history of UTI. If so, you’ll want to include diagnosis Z87.440 (Personal history of urinary (tract) infections) — and incorporate appropriate measures into the resident’s care plan.
Note: All of these diagnoses are “Return to Provider.”
All of these could, after testing, result in a definitive diagnosis. But you’ll need to find other codes once your provider pins down the specific UTI.
Tip 2: Investigate Other Sites, Names
As noted above, residents might have UTI symptoms that stem from other anatomic sites instead of the urinary tract. If you learn this is the case, the condition goes by a different name based on the specific site of the urinary infection: the kidneys (pyelonephritis), the bladder (cystitis), or the urethra (urethritis).
Because of the specific locations within the urinary tract, you’ll also find different diagnostic codes for infection in these locations; all of the following diagnoses qualify as “Acute Infections” or “Medical Management”:
Important: The N99 codes are complication codes, and they require physician documentation and confirmation of a cause-and-effect relationship between any specified procedure and the complicated condition.
Tip 3: Determine Whether Chronic or Acute
Another important consideration when selecting the final diagnosis is whether the resident’s condition is chronic (persistent) or acute (sudden, short-term).
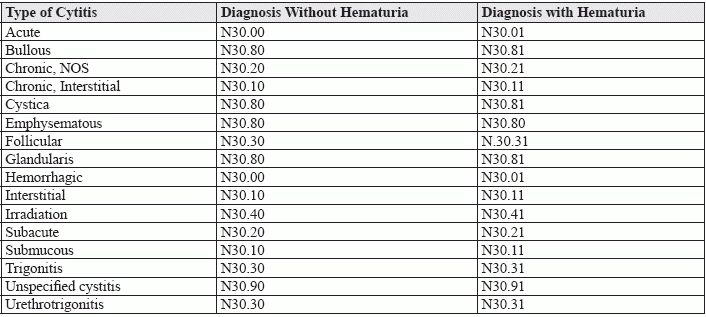
Example: If the resident has acute cystitis, you’ll report N30.0- (Acute cystitis), but if the resident’s cystitis is chronic, you’ll report N30.1- (Interstitial cystitis (chronic)) or N30.2- (Other chronic cystitis).
You might also need to report an additional code to identify the infectious agent (if applicable), reminds Michael A. Ferragamo, MD, FACS, clinical assistant professor of urology, State University of New York Stony Brook. If so, you’ll find the appropriate diagnoses in categories B95 through B97, which represent bacterial and viral infectious agents, and all of which are classified as “Acute Infections”:
Tip 3: Look for Hematuria
One last detail you’ll need to check in the physician’s documentation is whether they note that the resident also has hematuria. If the resident does, your coding will change.
Remember, however, that diagnosis N39.0 is an unspecified code. Ferragamo warns that many such diagnostic codes often lead to denials of claims by carriers when you report only unspecified ICD-10-CM diagnostic codes.
Bottom line: Strive for specificity, and don’t be afraid to query the physician if the documentation isn’t clear enough to support a definite diagnosis.
