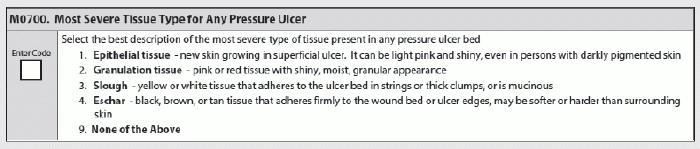
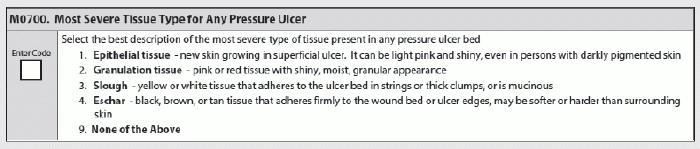
Coding M0700 — Most Severe Tissue Type for Any Pressure Ulcer is not always easy, especially when you have a wound that displays more than one tissue type. Learn from these scenarios to make your coding easier.
Scenario 1: A Stage 2 pressure ulcer is noted to have light pink, shiny tissue becoming visible in the wound.
How to code: The correct coding for M0700 in this scenario would be 1 — Epithelial tissue, answered Jennifer Pettis, RN, BS, WCC, consultant for the CMS Division of Nursing Homes, in the March 20 provider update presentation.
Explanation: “Epithelial tissue is new skin that is light pink and shiny, even in persons with darkly pigmented skin,” Pettis noted. “In Stage 2 pressure ulcers, epithelial tissue is seen in the center and edges of the wound, whereas in full-thickness Stage 3 and 4 pressure ulcers, epithelial tissue advances from the edges of the wound.”
When to Code ‘None of the Above’
Scenario 2: A pressure ulcer presents as a purple area of discolored skin. The area is boggy and warmer than the surrounding tissue.
How to code: This scenario describes suspected deep tissue injury (SDTI), Pettis said. And because none of the tissue types presented in M0700 apply to SDTI, you must code 9 — None of the Above.
You might also code 9 in other cases, such as for a Stage 1 pressure ulcer or a Stage 2 ulcer with an intact blister, Pettis noted. Code 9 as well for unstageable pressure ulcers, related either to a non-removable dressing or device, or to SDTI. You would code 9 in these instances because you cannot visualize the wound bed and therefore cannot assess it.
What to Do When an Ulcer Has Different Tissue Types
Scenario 3: A Stage 3 pressure ulcer on the sacrum presents with red bumpy tissue that has filled 75 percent of the ulcer and with light pink tissue that has resurfaced 25 percent of the ulcer.
How to code: You’re dealing with two tissue types here: the light pink tissue sounds like epithelial tissue, and the red bumpy tissue in the Stage 3 ulcer meets the definition of granulation tissue, said Lori Grocholski, MSW, LCSW, with CMS’s Center for Clinical Standards and Quality, in the provider update video.
In this scenario, the correct coding for M0700 is 2 — Granulation tissue, Grocholski stated. You can code granulation tissue if the wound is free of slough/eschar and contains granulation tissue, which is red tissue with a cobblestone or bumpy appearance. Also, granulation tissue bleeds easily when injured.
Scenario 4: A Stage 4 pressure ulcer has 25 percent black hard tissue present, 75 percent bumpy red tissue present, and scant epithelialization at the edges of the wound.
How to code: In this case, the correct coding is 4 — Eschar, Grocholski instructed. “Eschar is dead or devitalized tissue that is hard or soft in texture, usually black, brown or tan in color, and may appear scab-like.” Eschar is usually firmly adherent to the wound’s base and often the sides or edges.
Even though there is less eschar present in the wound than granulation tissue, eschar is the answer here because it is the most severe tissue type in the wound, Grocholski noted.
Scenario 5: A Stage 3 pressure ulcer is covered with 75 percent granulation and contains yellow, stringy tissue covering approximately 25 percent of the ulcer.
How to code: The yellow, stringy tissue meets the description of code 3 — Slough, Grocholski said. Slough is non-viable tissue that is usually moist and can be soft, stringy and mucinous in texture.
Slough can be one of several colors, including yellow, tan, gray, green or brown, Grocholski noted. “Slough may be adherent to the base of the wound or present in clumps throughout the wound.” So because slough is a more severe tissue type than granulation, you would code 3.