MDS Alert
Know Which Assessments Should Be on Your Radar
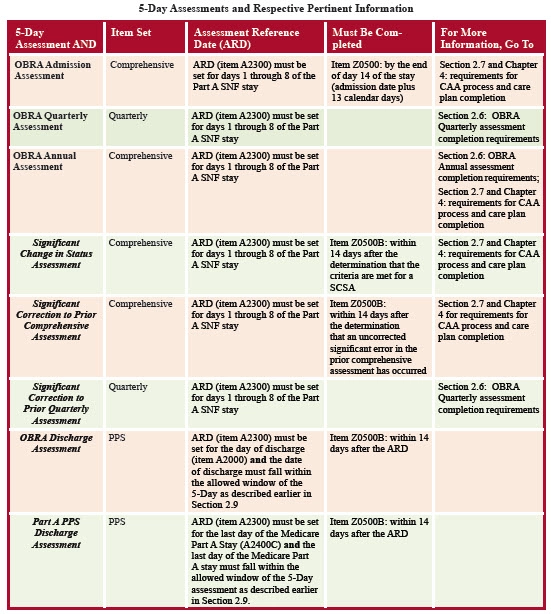
Keep these handy charts to differentiate various MDS assessments. Nurse assessment coordinators (NACs) and other professionals responsible for completing the Minimum Data Set (MDS) know that assessments constitute a huge part of the job — but keeping the various assessments straight is a job in and of itself. In the past couple years, there have been some major changes to how nursing homes are paid for the care they provide, and so some aspects of assessments have changed as well. Generally, there are fewer assessments required now. “Remember, the only folks doing the 14, 30, etc., are state Medicaid reimbursement programs still using RUG-III or RUG-IV,” says Jane Belt, MS, RN, QCP, RAC-MT, RAC-MTA, curriculum development specialist at American Association of Post-Acute Care Nursing (AAPACN) in Denver. “As of Oct. 1, 2020, states can opt to do the state PDPM assessment if the state wants to collect that data for future payment models,” Belt says. Catch Up on This Background There are a lot of acronyms to understand, and it’s helpful to know which payment systems are (or were) used when. “Over half of the State Medicaid programs also use the MDS for their case-mix payment systems. The Resource Utilization Group, Version IV (RUG-IV) system replaced the Resource Utilization Group, Version III (RUG-III) system for Medicare starting on October 1, 2010. Starting October 1, 2019, PDPM replaced the RUG-IV system. However, State Medicaid agencies have the option to use the RUG-III, RUG-IV, or PDPM classification systems,” says the Resident Assessment Instrument (RAI) Manual on page 6-2. A lot of the information you’re responsible for compiling and submitting is state dependent, so make sure you reach out to your respective state or region Medicare and Medicaid agencies for specifics. “States have the option of selecting the system (RUG-III or RUG-IV) with the number of Rehabilitation groups that better suits their Medicaid long-term care population. State Medicaid programs always have the option to develop nursing home reimbursement systems that meet their specific program goals. The decision to implement a certain classification system for Medicaid is a State decision. Please contact your State Medicaid agency if you have questions about your State Medicaid reimbursement system,” the RAI Manual says. Clip and Save These Charts Keep these tables handy either to get the hang of the assessment process and timeline or as a quick reference! The SNF Prospective Payment System (PPS) has a schedule of PPS assessments, which center around the 5-Day assessment. “The 5-Day assessment is the only required PPS assessment that is used to support PPS reimbursement. However … an optional assessment, the Interim Payment Assessment (IPA), may be used to reclassify the resident into a new PDPM classification, and would also affect the associated payment,” the RAI Manual says on page 6-2. “The ARD for the IPA is determined by the provider, and the assessment period is the last 3 days (i.e., the ARD and the 2 calendar days prior). It is important to note that the IPA changes payment beginning on the ARD and continues until the end of the Medicare Part A stay or until another IPA is completed. The IPA does not affect the variable per diem schedule,” the RAI Manual says, in various places.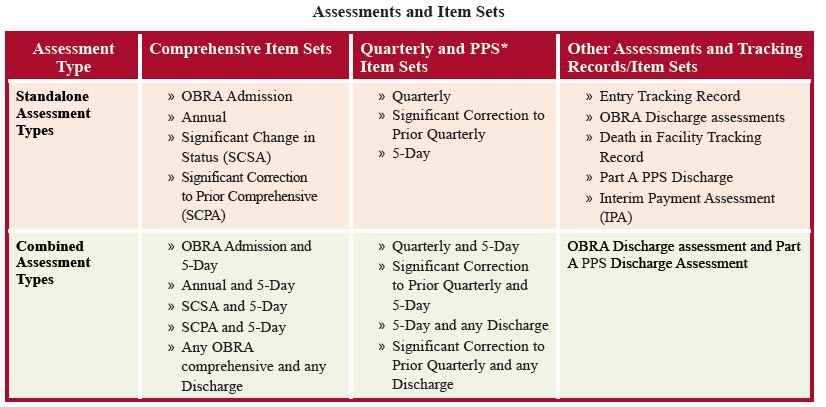
MDS Alert
- COVID-19:
Understand How Vaccinations Affect Visitation
Don’t expect “normal,” but hope is on the horizon. Although some long-term care facilities are [...] - Workplace Safety:
Be Prepared for More Intensive SNF, NF Scrutiny
Know what federal agencies and Congress are looking into. The Occupational Health and Safety Administration [...] - Back to Basics:
Know Which Assessments Should Be on Your Radar
Keep these handy charts to differentiate various MDS assessments. Nurse assessment coordinators (NACs) and other [...] - Reader Questions:
Brush Up On What Other Credentials ‘Physician’ Includes
Question: When I’m working on the Minimum Data Set (MDS), what does the word “physician” [...] - Reader Questions:
Know These Facts About Optional State Assessments
Question: How is the Optional State Assessment (Item A0300) different from the other assessments I [...] - Reader Questions:
Don’t Mix Vaccination Records
Question: I work at an independent skilled nursing facility, the only one in my rural [...]

