MDS Alert
3 Examples Show You How To Count Therapy In Look-Back Period
When the Centers for Medicare & Medicaid Services (CMS) added the new MDS 3.0 item O0420 — Distinct Calendar Days of Therapy, you didn’t simply get an additional item to code in the MDS. In fact, the addition of O0420 has further and far-reaching implications for calculating classification into the Medicare Rehabilitation Medium and Low RUG-IV categories.
Simply stated, item O0420 requires that you report the distinct calendar days of therapy provided. “Distinct calendar days represents the different days therapy was provided in the assessment reference date (ARD) or change of therapy (COT) review look-back period, wrote Kris Mastrangelo in a recent Harmony Healthcare International blog posting. “In other words, how many different days were rehabilitation services provided for greater than 15 minutes over the last seven days?”
Mastrangelo provided the following example:
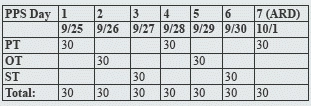
How to code: You would report this as:
-
Physical Therapy (PT) three days for a total of 90 minutes.
-
Occupational Therapy (OT) two days for a total of 60 minutes.
-
Speech Therapy (ST) two days for a total of 60 minutes.
-
Seven Distinct Calendar Days.
How Distinct Calendar Days Impacts Your RUG Classification
Old way: Before Oct. 1, 2013, the MDS RUG-IV Grouper allowed you to meet the classification criteria for the Medium Rehabilitation category without five distinct days of therapy, Mastrangelo noted.
New way: But now “the RUG-IV grouper will only calculate a Rehabilitation Medium RUG category when 150 minutes of therapy is provided across five distinct calendar days,” Mastrangelo said. This means that within the seven-day observation period of the MDS or COT review, therapists must deliver services to the patient on at least five or the seven days in the observation period from the ARD.
“If this criterion is not met, regardless of the number of minutes or total of combined discipline visits of rehabilitation services provided, the RUG score generated will reduce to a Nursing RUG,” Mastrangelo warned. Here’s the example:
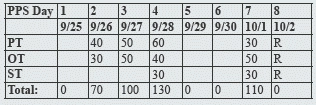
How to code: For this example, Mastrangelo instructed that you would code as follows:
-
PT four days for a total of 180 minutes.
-
OT four days for a total of 170 minutes.
-
ST two days for a total of 60 minutes.
-
Four Distinct Calendar Days.
“Although therapy was provided for a total of 10 visits, the Rehabilitation Medium criteria will not be met and a Nursing RUG classification will apply,” Mastrangelo noted. This would fall into the Rehabilitation Low categories, for which therapy must be provided on three or more distinct calendar days — only if there were two nursing restorative programs on at least six days during the look-back period.
Here is another example from a blog posting by Gina Tomcsik, director of compliance for Functional Pathways in Knoxville, TN:
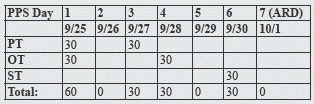
How to code: Prior to Oct. 1, 2013, this example would produce a Medium Rehabilitation RUG, counting as five days of therapy, Tomcsik explained. But under the new rules, the RUG would classify as Low Rehabilitation with four distinct days of therapy (again, with two nursing restorative programs on at least six days):
-
PT two days for a total of 60 minutes.
-
OT two days for a total of 60 minutes.
-
ST one day for a total of 30 minutes.
-
Four Distinct Calendar Days.
Keep in mind: The criteria for Ultra High, Very High, and High categories won’t change under the 2014 requirements, according to Mastrangelo. For RUG classification in these categories, at least one discipline must provide five days in the observation period in addition to meeting the criteria for total minutes.
MDS Alert
- Documentation:
Do Your Clinical Record & MDS Match Up For ADLs?
How to handle documentation when ADL levels change. Because the MDS is the basis for [...] - Section J:
Look For This Language In The Medical Record To Properly Code J1400
Follow 5 tips to determine correct coding for this item. If you’re poring over the [...] - Therapy:
How To Balance Therapy Days & RUG Categories
Don’t let a COT throw a wrench in your RUG classification. With all the recent [...] - MDS 3.0:
MDS Corrections: 8 Scenarios Show You The Way
Know when to complete an SCSA vs. an SCPA. After reviewing prior assessments and records, [...] - What Do You Think?
Question 1: I am still confused about when to do a Change in Therapy (COT). [...] - Industry News to Use:
What The OIG Has In Store For SNFs This Year
Plus: CDC launches new website just for LTC providers. Beware: The Centers for Medicare & [...] - 3 Examples Show You How To Count Therapy In Look-Back Period
When the Centers for Medicare & Medicaid Services (CMS) added the new MDS 3.0 item [...] - Clip 'N' Save:
Use This Tool To Double-Check Short-Stay Qualification
Get a helping hand to properly code Z0100C. When you’re coding item Z0100 — Medicare [...] - In other news:
Check Out This New LTC-Focused CDC Website If you’re looking for expert information and resources [...]

