Steer Clear Using O0700 Days as a RUG Enhancer
The last thing you want is to attract surveyors’ attention by getting Item O0700 — Physician Orders wrong. It might ratchet up your RUG categories, but is likelier to land your facility in hot water.
Beware of 2 Red Flags
Case in point: Louisiana’s recent Medicaid Case Mix Documentation Reviews revealed that facilities are obtaining physician orders solely for the purpose of meeting a particular RUG classification, according to a recent alert from the Louisiana Department of Health and Hospitals. Coding on the MDS Item O0700 indicated alterations to the count of days for physician orders to affect the RUG-III classification of an assessment and corresponding Medicaid case mix reimbursement.
Among the many suggestions in the list of coding tips for special populations (page O-45), the RAI Manual clearly highlights red flags for this practice:
Keep Your O0700 Coding Accurate
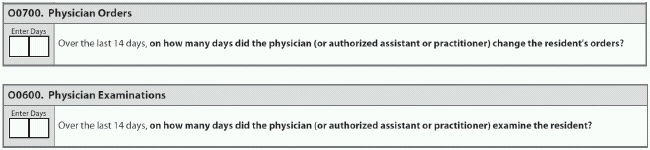
What to do: To avoid even the appearance of trying to erroneously boost your RUG classification, make sure that you begin your process of coding Item O0700 by reviewing the physician order sheets in the resident’s medical record. Then, enter the number of days in the last 14 days (or since admission if less than 14 days ago) that the physician has changed the orders.
Include in your count of days any written, telephone, fax or consultation orders for new or altered treatment, according to a recent training by the Ohio Department of Health (ODH) RAI Coordinator’s office.
Tip: Orders on the day of admission resulting from an unexpected change/deterioration or injury are considered new or altered orders — so be sure to count these as well.
Don’t Include These Orders Either
Mistake: According to a recent MDS training session by Shirley Boltz, RN, RAI/Education Coordinator for the Kansas Department for Aging and Disability Services (KDADS), do not include the following orders in Item O0700:
Standard admission, return admission, renewal or clarifications without changes;
And while you’re cleaning up your O0700 coding, you might as well make sure that your coding of Item O0600 — Physician Examinations is up to snuff.
For O0600, code the number of days during the 14-day look-back period (or since admission if less than 14 days ago) that the physician’s progress notes reflect that the physician examined the resident, Boltz instructed. The examination can occur in the facility, in the physician’s office, in a dialysis center, or via telehealth.
The evaluation may include a partial or a full exam, as well as monitoring the resident’s response to treatment and/or adjusting treatment as a result of the exam, Boltz noted. But the exam must be documented in the clinical record by the physician.
Physicians may include medical doctors, doctors of osteopathy, podiatrists, dentists, and authorized physician assistants, nurse practitioners or CNS working in collaboration with the physician, according to ODH.
Error: Do not include exams during emergency room visits or hospital observation stays, or exams prior to admission/reentry, Boltz warned.