Long-Term Care Survey Alert
Know When Shortness of Breath Is Indicative of a Change In Condition
Hint: Watch resident’s behavior to identify whether it is a current issue.
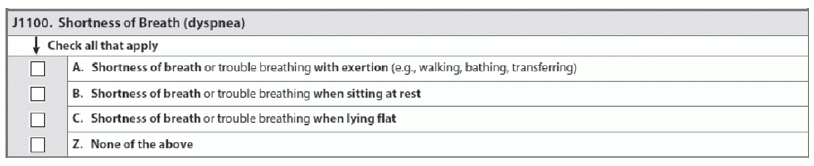
Coding Item J1100 — Shortness of Breath (dyspnea) correctly is not as simple as it seems. You’ll need to specify what the patient is doing that is causing this condition and pay attention to any new symptoms that could indicate a new underlying problem.
Why Correct J1100 Coding is So Important
Experiencing shortness of breath or trouble breathing can be distressing for residents, and it can cause decreased interaction, activity and quality of life, according to a recent training presentation by Shirley Boltz, RN, RAI Education Coordinator for the Kansas Department for Aging and Disability Services (KDADS). Additionally, if a resident begins to experience shortness of breath, this is a potential indication of a change in condition.
There are many ways to find evidence of breathing trouble, including reviewing the medical record and interviewing the resident, staff and family members. But beware that residents sometimes don’t tell staff or family members about their shortness of breath, so that’s why it’s important to ask staff about any observations of breathing difficulties.
Residents will also often avoid activities that cause them shortness of breath to prevent breathing difficulties. These are all clues that will lead to accurate coding of Item J1100.
When to Code Each J1100 Sub-Item
According to Boltz, Item J1100 has a seven-day look-back period and three basic coding choices to record shortness of breath or trouble breathing:
Simply put, you should check J1100A if the resident has shortness of breath or trouble breathing when he is engaging in activity, according to the Oklahoma State Department of Health (OSDH) Quality Improvement & Evaluation Service.
And keep in mind that this could be any type of activity — shortness of breath could be present during an activity as limited as turning or moving in bed during daily care, or with more strenuous activity such as transferring, walking, or bathing, the OSDH said. “If the resident avoids activity or is unable to engage in activity because of shortness of breath, then code this as present.”
Conversely, you should check J1100B if the resident experiences shortness of breath or trouble breathing when he is sitting at rest. Check J1100C when the resident has problems breathing when he attempts to lie flat, OSDH instructed. “Also code this as present if the resident avoids lying flat because of shortness of breath.”
Finally, if the resident reports no shortness of breath or trouble breathing, and the medical record and staff interviews indicate that shortness of breath appears to be absent or well controlled with current medication, check J1100Z — None of the above, OSDH said.
Check All that Apply
In many cases, the resident may experience shortness of breath or trouble breathing in more than one of the scenarios described in Item J1100. The OSDH provides the following example:
Scenario: Mrs. W. has a diagnosis of chronic obstructive pulmonary disease (COPD) and heart failure. She is on two liters of oxygen and daily respiratory treatments. With oxygen, she is able to ambulate and participate in most group activities, but she reports feeling “winded” when walking the length of the hallway or going to the dining room.
Staff have observed Mrs. W. having to stop and rest several times, and recently, she describes feeling “out of breath” when she tries to lie down.
How to code: Because Mrs. W. reported being short of breath when lying down, as well as during walking that required ambulating longer distances, you would check both J1100A and J1100C.
Long-Term Care Survey Alert
- Survey Strategies:
Tap This Insider Tool to Improve Dementia Care -- or Invite Survey Citations
CMS worksheet reveals clues to compliance in 2016. What began as a five-state dementia care [...] - Toolkit:
Take Advantage of This Dementia Care Guidance
If your facility does not yet plan care according to nationally accepted dementia care guidelines, [...] - Reimbursement:
Recognize What Earns a Special Care High RUG
Take note of when a resident would classify as Clinically Complex, not Special Care High. [...] - Section J:
Know When Shortness of Breath Is Indicative of a Change In Condition
Hint: Watch resident’s behavior to identify whether it is a current issue. Coding Item J1100 [...] - Heads Up:
CMS Posts New Draft MDS 3.0 Item Sets & Data Specs
You can now get a sneak peek at the draft versions of the MDS 3.0 [...]

