Long-Term Care Survey Alert
Get a Handle On The Most Significant MDS Changes
Are you certain about what an ‘episode of care’ signifies?
If you’ve been struggling to absorb the updates made recently in the RAI Manual v1.12, here’s some expert advice and instruction to help you grasp the crucial Chapter 3 changes.
Learn What A0310B Selection Deletion Means
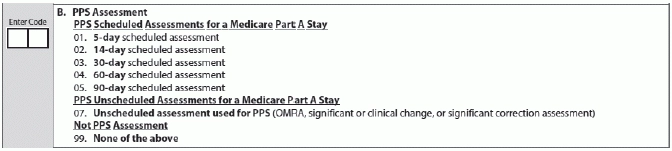
A0310B — PPS Assessment is a subset of MDS items used for payment and quality measures, according to MDS education coordinator Mary Mass in a recent presentation for the North Carolina Department of Health and Human Services, Division of Health Service Regulation. The assessment reference date (ARD) is the key date and you must set it within a pre-determined window.
The first day of the Medicare Part A coverage for the current stay is considered Day 1 for PPS scheduling purposes, Mass explained. Remember that “grace days” are a Medicare-only concept, and do not transmit assessments that are not Medicare.
New: Under A0310B, the RAI Manual update deletes from the MDS assessments selection 06 — Readmission/return assessment. Instead, you’ll use the five-day scheduled assessment for all Medicare admissions and readmissions/returns, stated Springfield, MO-based managing healthcare consultant Suzy Harvey in an October 2014 analysis for BKD, LLP.
Understand These A0410 Changes
A0410 — Unit Certification or Licensure Designation designates the submission authority for the resident assessment, Mass said. This is based on the bed status, not on the resident’s payer source.
During a recent Centers for Medicare & Medicaid Services (CMS) Skilled Nursing Facility (SNF) Open Door Forum, participants made several comments concerning the RAI guidelines for coding 3 — Unit is Medicare and/or Medicaid certified, Harvey noted. “There was much confusion, as the guidelines found in Chapter 3 of the RAI manual state if the resident is in a Medicare- and/or Medicaid-certified bed, regardless of payer source, the facility is required to submit these MDS records to the Quality Improvement and Evaluation System (QIES) Assessment Submission and Processing (ASAP) system.”
“Chapter 5 states — and CMS confirmed — assessments completed for purposes other than the Omnibus Budget Reconciliation Act (OBRA) and skilled nursing facility prospective payment system (SNF PPS) are not to be transmitted,” Harvey said. “This includes assessments completed for Medicare Advantage, Managed Care and private insurance.”
Beware: You can change A0410 only with a manual correction/deletion request form submitted to your state agency, Mass stated.
Chapter 5, page 13 of the RAI Manual states: “A QIES ASAP system record with an incorrect submission requirement in item A0410 is a very serious problem. Submission of MDS assessment records to the QIES ASAP system constitutes a release of private information and must conform to privacy laws.”
You cannot use a modification or inactivation request to correct the A0410 value, because a copy of the record in error will remain in the QIES ASAP system history file where there is both federal and state access to the record, Mass cautioned.

Know How New Item A1900 Impacts Other Items
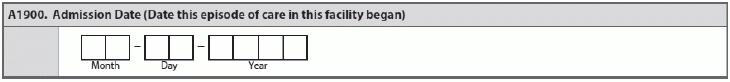
A1900 — Admission Date is a new item that CMS added to the MDS. “The admission date for coding Item A1900 is the date the current ‘episode of care’ in the facility began,” Harvey explained. “Neither CMS nor the RAI Manual provides clear guidance on the definition of ‘episode of care.’”
“Based on the software development/vendor call with CMS in January 2014, the definition is the same as in the Quality Measures manual, which says an episode is a series of one or more stays that may be separated by brief interruptions in the resident’s time in the facility,” Harvey noted. “The episode of care definition also mirrors the 90-plus days of episode of care from the Program for Evaluating Payment Patterns Electronic Reports (PEPPER). Further clarification from CMS is pending.”
In the case of a discharge return anticipated where the resident returns within 30 days, you would change the Entry Date at A1600, but not the Admission Date at A1900, Mass explained.
For A2000 — Discharge Date, you enter the date the resident leaves the facility. The discharge date and the ARD must be the same for Discharge assessments, Mass reminded. But the discharge date may be later than the end of the Medicare stay date if the resident is receiving services under the SNF Part A PPS and remains in the facility in a certified bed after decertified from the Part A stay. Do not include LOAs.
Adjust the ARD (A2300) to equal the discharge date only if the resident dies or is discharged prior to the end of the look-back period, Mass said. Remember that all MDS sections must use the same ARD and you cannot change it after your complete the assessment.
Link: To view the new RAI Manual v1.12, go to www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/MDS30RAIManual.html. Scroll down to the “Downloads” section at the bottom of the page to access links to RAI Manual chapters, MDS 3.0 sections and appendices.
Long-Term Care Survey Alert
- Emergency Readiness Planning:
Make "Be Prepared" This New Year's Resolution
Beware survey-related snafus if you aren’t ready. 2014 brought news of several tragic nursing home [...] - Compliance:
Avoid a Survey Crisis
Ensure your emergency plan supports regulatory requirements. Make no mistake. Some aspects of emergency preparedness [...] - Quality of Care:
Watch Out: Crack Down on Nursing Home Quality-Of-Care Likely In 2015
Don’t let staffing issues become your Achilles’ heel. You can expect unprecedented scrutiny of your [...] - Section A:
Get a Handle On The Most Significant MDS Changes
Are you certain about what an ‘episode of care’ signifies? If you’ve been struggling to [...] - HIPAA Compliance:
Don't Let Emergencies Become a HIPAA Breach Disaster
Least possible information is the gold standard. Remember your obligations to public health reporting don’t [...] - Check Out 3 Important RAI Manual Technical Updates
The Centers for Medicare & Medicaid Services (CMS) made several key changes to the RAI [...]

